Ileocecal Tuberculosis: A case report
DOI:
https://doi.org/10.22516/25007440.515Keywords:
Ileocecal tuberculosis, intestinal tuberculosis, extrapulmonary tuberculosis. PCR for Mycobacterium Tuberculosis, splenic infarction, bone tuberculosisAbstract
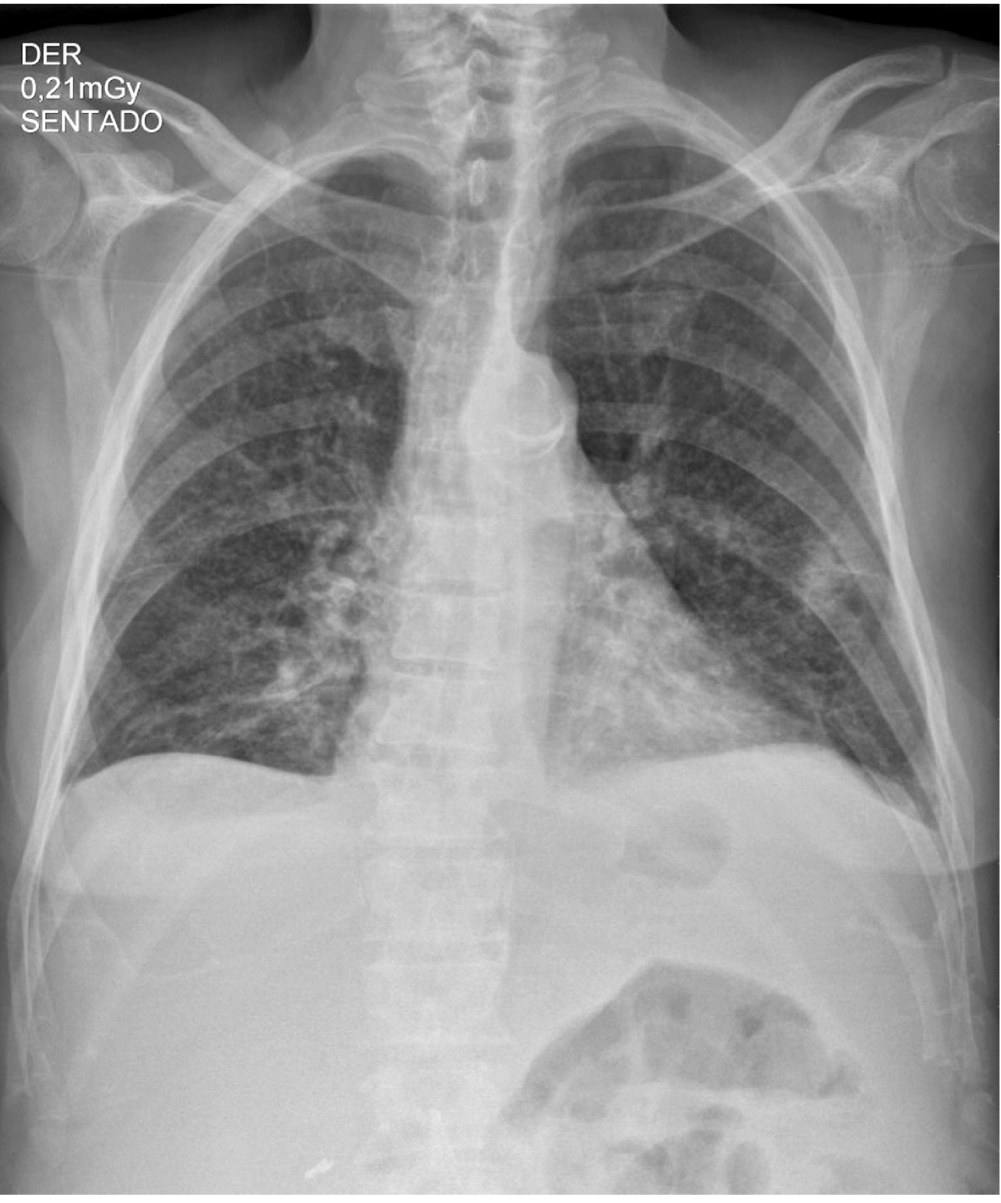
Tuberculosis is a disease of global public health importance, with a high incidence at the lovel of Colombian territory. It mainly affects lung parenchyma, however, in a high percentage of cases, it is diagnosed in its extrapulmonary form being the gastrointestinal tract one of the most frecuent sites. Also the ileocecal región and the terminal ileum are the regions with the most predilection for the Mycobaterium Tuberculosis bacteria. The manifestations in this rare presentation of the disease are given by abdominal pain and sensation of mass mainly, ulcerative lesions in the intestinal mucosa and histological findings corresponding to large caseificant granulomas and confluent morphology, differentiating from other entities like Crohn’s Disease. The search for the disease within the gastrointestinal tract will be carried out with the help of invasive methods such as colonoscopy and laboratory diagnostic aids such as cultures, stains or PCR. Given the complexity of diagnosing in this form of Tuberculosis, the knowledge and the way in which a patient with a suggestive picture of the disease is approached are important factors in establishing the timely therapeutic management. We share an unusual ileocecal - TBC case as a manifestation of prolonged febrile symdrome with fatal outcome.
Downloads
References
MacNeil A, Glaziou P, Sismanidis C, Maloney S, Floyd K. Global Epidemiology of Tuberculosis and Progress Toward Achieving Global Targets - 2017. MMWR Morb Mortal Wkly Rep. 2019;68(11):263-266. https://doi.org/10.15585/mmwr.mm6811a3
Pérez MPL. Informe de evento tuberculosis, Colombia, 2017. 2018;(03):21.
Narasimhan P, Wood J, Macintyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:828939. https://doi.org/10.1155/2013/828939
Gupta RK, Lucas SB, Fielding KL, Lawn SD. Prevalence of tuberculosis in post-mortem studies of HIV-infected adults and children in resource-limited settings: a systematic review and meta-analysis. AIDS. 2015;29(15):1987-2002. https://doi.org/10.1097/QAD.0000000000000802
Peirse M, Houston A. Extrapulmonary tuberculosis. Medicine. 2017;45(12):747-52. https://doi.org/10.1016/j.mpmed.2017.09.008
Stewart RJ, Tsang CA, Pratt RH, Price SF, Langer AJ. Tuberculosis - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(11):317-323. https://doi.org/10.15585/mmwr.mm6711a2
Debi U, Ravisankar V, Prasad KK, Sinha SK, Sharma AK. Abdominal tuberculosis of the gastrointestinal tract: revisited. World J Gastroenterol. 2014;20(40):14831-40. https://doi.org/10.3748/wjg.v20.i40.14831
Ramírez-Lapausa M, Menéndez-Saldaña A, Noguerado-Asensio A. Tuberculosis extrapulmonar, una revisión. Rev Esp Sanid Penit. 2015;17(1):3-11. https://doi.org/10.4321/S1575-06202015000100002
Zuluaga M. Tuberculosis intestinal: un diagnóstico para no olvidar. Reporte de un caso. Med U.P.B. 2015;34(2):165-170. https://doi.org/10.18566/%20medupb.v34n2.a10
Cho JK, Choi YM, Lee SS, Park HK, Cha RR, Kim WS, Kim JJ, Lee JM, Kim HJ, Ha CY, Kim HJ, Kim TH, Jung WT, Lee OJ. Clinical features and outcomes of abdominal tuberculosis in southeastern Korea: 12 years of experience. BMC Infect Dis. 2018;18(1):699. https://doi.org/10.1186/s12879-018-3635-2
Donoghue HD, Holton J. Intestinal tuberculosis. Curr Opin Infect Dis. 2009;22(5):490-6. https://doi.org/10.1097/QCO.0b013e3283306712
Patel B, Yagnik VD. Clinical and laboratory features of intestinal tuberculosis. Clin Exp Gastroenterol. 2018;11:97-103. https://doi.org/10.2147/CEG.S154235
Malikowski T, Mahmood M, Smyrk T, Raffals L, Nehra V. Tuberculosis of the gastrointestinal tract and associated viscera. J Clin Tuberc Other Mycobact Dis. 2018;12:1-8. https://doi.org/10.1016/j.jctube.2018.04.003
Rathi P, Gambhire P. Abdominal Tuberculosis. J Assoc Physicians India. 2016;64(2):38-47.
da Rocha EL, Pedrassa BC, Bormann RL, Kierszenbaum ML, Torres LR, D’Ippolito G. Abdominal tuberculosis: a radiological review with emphasis on computed tomography and magnetic resonance imaging findings. Radiol Bras. 2015;48(3):181-91. https://doi.org/10.1590/0100-3984.2013.1801
Pulimood AB, Amarapurkar DN, Ghoshal U, Phillip M, Pai CG, Reddy DN, Nagi B, Ramakrishna BS. Differentiation of Crohn’s disease from intestinal tuberculosis in India in 2010. World J Gastroenterol. 2011;17(4):433-43. https://doi.org/10.3748/wjg.v17.i4.433
Gutiérrez O, Estay R, Cerda C, Capona R. Tuberculosis ileocecal: revisión de la literatura a partir de un caso clínico. Gastroenterol Latinoam. 2016;27(1):31-36.
Kivihya-Ndugga L, van Cleeff M, Juma E, Kimwomi J, Githui W, Oskam L, Schuitema A, van Soolingen D, Nganga L, Kibuga D, Odhiambo J, Klatser P. Comparison of PCR with the routine procedure for diagnosis of tuberculosis in a population with high prevalences of tuberculosis and human immunodeficiency virus. J Clin Microbiol. 2004;42(3):1012-5. https://doi.org/10.1128/jcm.42.3.1012-1015.2004
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















