Criterios ASGE 2010 frente a 2019 para coledocolitiasis en pacientes llevados a colangiopancreatografía retrógrada endoscópica
DOI:
https://doi.org/10.22516/25007440.883Palabras clave:
Coledocolitiasis, Colangiopancreatografía Retrógrada Endoscópica, Sistemas de SaludResumen
Introducción: con la actualización de las guías de la American Society for Gastrointestinal Endoscopy (ASGE) 2019, los criterios para los pacientes con sospecha de coledocolitiasis se volvieron más estrictos a la hora de elegir quienes deben ser llevados directamente a colangiopancreatografía retrógrada endoscópica (CPRE). El objetivo de este estudio fue comparar a los pacientes llevados directamente a CPRE según las guías ASGE de 2010 frente a la guía de 2019.
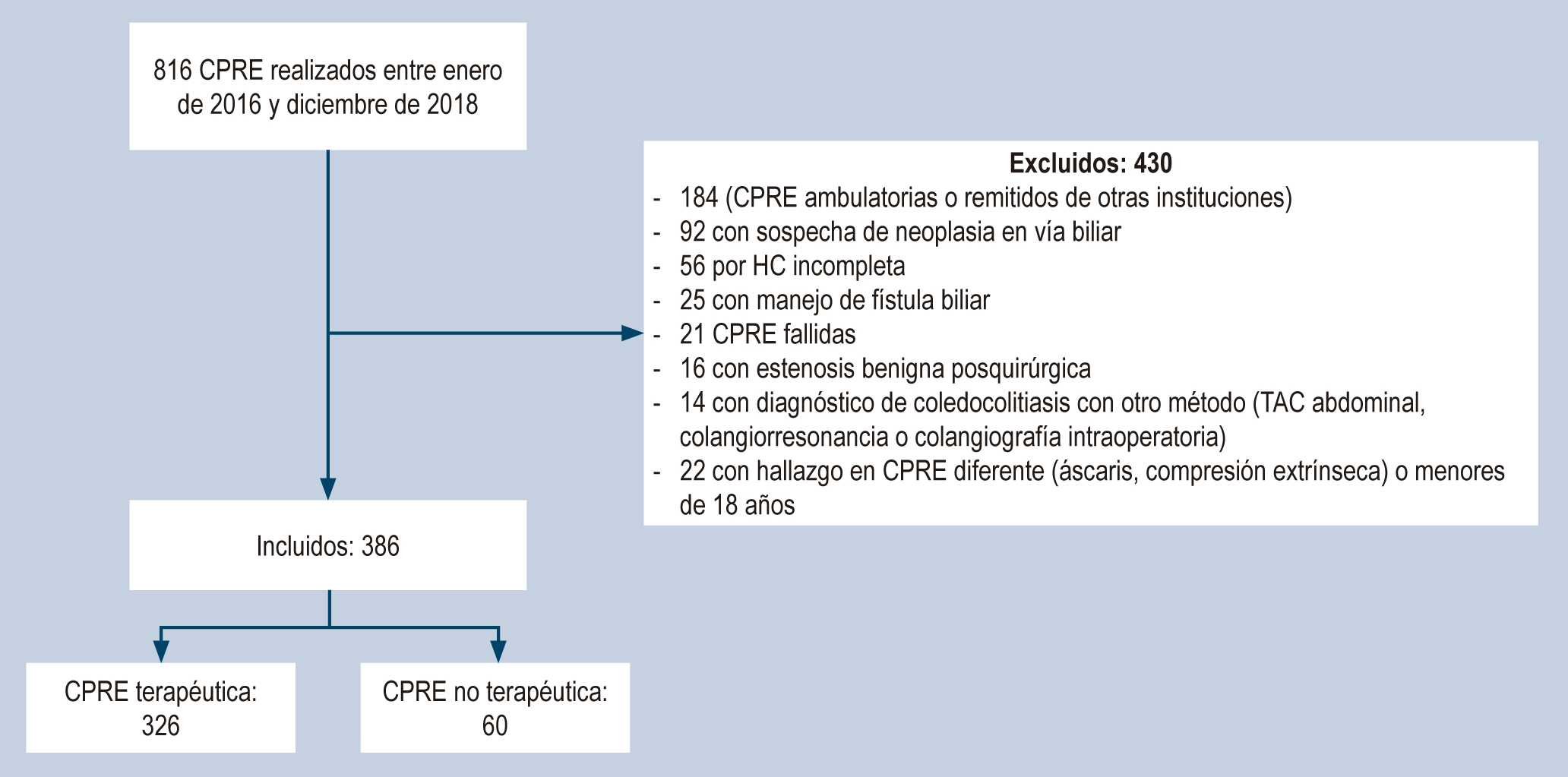
Métodos: estudio retrospectivo de las CPRE realizadas entre enero de 2016 y diciembre de 2018 que evaluó el rendimiento diagnóstico de las variables paraclínicas y ecográficas de forma individual y en conjunto para comparar su sensibilidad, especificidad, valores predictivos y precisión de la probabilidad alta según guías de 2019 y de 2010 respecto a la presencia de cálculos en las CPRE.
Resultados: 386 pacientes se llevaron a CPRE por sospecha de coledocolitiasis, 84,5% fueron procedimientos terapéuticos. El grupo de probabilidad alta presentó mayor tasa de CPRE terapéutico: 89,3% según las guías de 2019 frente a las de 2010 con 86,3% (p < 0,001). La sensibilidad y especificidad de la probabilidad alta según las guías de 2010 fueron del 86,8% y 25,0%, respectivamente, con un valor predictivo positivo (VPP) del 86,3% y una precisión del 77,2%. La probabilidad alta según las guías de 2019 mostró una menor sensibilidad (74%), pero mayor especificidad (51,7%), un VPP del 89,3% y una precisión del 70,7%.
Conclusiones: la implementación de las guías ASGE 2019 sobre las indicaciones para la realización de la CPRE debe considerarse teniendo en cuenta los recursos de los centros hospitalarios, sobre todo en países de bajos y medianos ingresos. Las guías ASGE 2010 presentan una buena sensibilidad y precisión para orientar la realización de la CPRE.
Descargas
Referencias bibliográficas
ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9. https://doi.org/10.1016/j.gie.2009.09.041
He H, Tan C, Wu J, Dai N, Hu W, Zhang Y, et al. Accuracy of ASGE high-risk criteria in evaluation of patients with suspected common bile duct stones. Gastrointest Endosc. 2017;86(3):525-32. https://doi.org/10.1016/j.gie.2017.01.039
Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, et al. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88-93. https://doi.org/10.1016/j.gie.2014.12.023
Sethi S, Wang F, Korson AS, Krishnan S, Berzin TM, Chuttani R, et al. Prospective assessment of consensus criteria for evaluation of patients with suspected choledocholithiasis. Dig Endosc Off J Jpn Gastroenterol Endosc Soc. 2016;28(1):75-82. https://doi.org/10.1111/den.12506
Ripari G, Wulfson A, Guerrina C, Perroud H. Correlación entre predictores de litiasis coledociana y los hallazgos en la colangiopancreatografía retrógrada endoscópica. Acta Gastroenterol Latinoam. 2017;47(4):269-76.
Rubin MIN, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2013;45(9):744-9. https://doi.org/10.1016/j.dld.2013.02.005
Gómez Hinojosa P, Espinoza-Ríos J, Bellido Caparo A, Pinto Valdivia JL, Rosado Cipriano M, Prochazka Zarate R, et al. Precisión de los predictores de la ASGE en el diagnóstico de coledocolitiasis en un hospital público de Lima, Perú. Rev Gastroenterol Perú. 2018;38(1):22-8.
ASGE Standards of Practice Committee, Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89(6):1075-1105.e15. https://doi.org/10.1016/j.gie.2018.10.001
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781-8. https://doi.org/10.1111/j.1572-0241.2007.01279.x
Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepato-Biliary-Pancreat Sci. 2018;25(1):17-30. https://doi.org/10.1002/jhbp.515
Chandran A, Rashtak S, Patil P, Gottlieb A, Bernstam E, Guha S, et al. Comparing diagnostic accuracy of current practice guidelines in predicting choledocholithiasis: outcomes from a large healthcare system comprising both academic and community settings. Gastrointest Endosc. 2021;93(6):1351-9. https://doi.org/10.1016/j.gie.2020.10.033
Hasak S, McHenry S, Busebee B, Fatima S, Sloan I, Weaver M, et al. Validation of choledocholithiasis predictors from the «2019 ASGE Guideline for the role of endoscopy in the evaluation and management of choledocholithiasis.» Surg Endosc. 2022;36(6):4199-206. https://doi.org/10.1007/s00464-021-08752-z
Jacob JS, Lee ME, Chew EY, Thrift AP, Sealock RJ. Evaluating the Revised American Society for Gastrointestinal Endoscopy Guidelines for Common Bile Duct Stone Diagnosis. Clin Endosc. 2021;54(2):269-74. https://doi.org/10.5946/ce.2020.100
Montoya-Botero J, Oliveros-Wilches R, Abadía-Díaz M, Sánchez-Pedraza R, Garrido-Bohórquez A de J, Manrique-Acevedo ME, et al. Colangiopancreatografía retrógrada endoscópica en una institución de referencia en cáncer. Rev Colomb Gastroenterol. 2020;35(4):430-5. https://doi.org/10.22516/25007440.512
Garcés Otero JS, Mejía Henao PA, Uribe A, Serrano Otero JA, Velásquez A, Agudelo Posada JJ, et al. Complicaciones y factores de riesgo en pacientes sometidos a colagiopancreatografía retrógrada endoscópica en una clínica de tercer nivel de Medellín desde el 2014 hasta el 2017. Rev Colomb Cir 2020;35(1):57-65. https://doi.org/10.30944/20117582.588
Lee HJ, Cho CM, Heo J, Jung MK, Kim TN, Kim KH, et al. Impact of Hospital Volume and the Experience of Endoscopist on Adverse Events Related to Endoscopic Retrograde Cholangiopancreatography: A Prospective Observational Study. Gut Liver. 2020;14(2):257-64. https://doi.org/10.5009/gnl18537
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


















