Challenges in the Diagnosis of Gastroparesis: Divergence Between Gastric Emptying Scintigraphy Results for Liquids and Solids
DOI:
https://doi.org/10.22516/25007440.1228Keywords:
Gastroparesis, gastric emptying, Scintigraphy, FoodAbstract
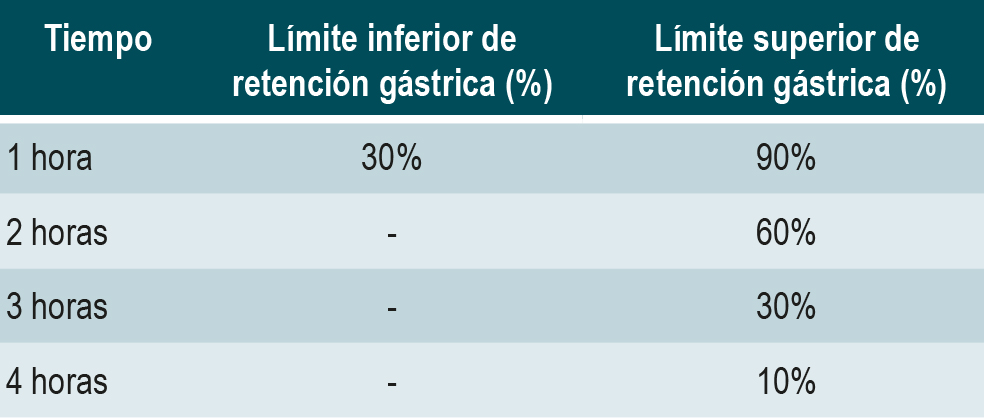
Introduction: Gastric emptying scintigraphy with solid food is the recommended gold standard for studying gastroparesis in patients after mechanical obstruction has been ruled out, according to the latest clinical guidelines. Although gastric emptying for liquids can also be assessed, the results of these two phases may not always align.
Objective: To determine the level of concordance between gastric emptying scintigraphy results for solids and liquids in the evaluation of gastroparesis at three nuclear medicine centers in Bogotá, Colombia.
Methodology: Data from all patients who underwent both phases of the study were reviewed. Patients under 18 years of age, those with accelerated results in either phase, or those with incomplete data were excluded. Cohen’s kappa coefficient was calculated to assess agreement between the tests. A bivariate analysis was performed to examine the association between test results, the level of agreement, and sociodemographic and clinical variables.
Results: A total of 210 patients met the inclusion criteria. Delayed results were observed in the solid phase in 86 patients (41%) and in the liquid phase in 181 patients (86%). The kappa value was κ = 0.082 (95% confidence interval [CI]: 0.005–0.16), with statistically significant results (p < 0.05). The most common pattern of divergence was normal solid-phase emptying with delayed liquid-phase emptying, observed in 102 patients (48.6%).
Conclusion: The level of concordance between gastric emptying scintigraphy for liquids and solids is low. The solid phase is considered the gold standard, and the results of the liquid phase should be interpreted with caution, taking into account the clinical context of each patient.
Downloads
References
Bharucha AE. Epidemiology and Natural History of Gastroparesis. Gastroenterol Clin North Am. 2015;44(1):9-19. https://doi.org/10.1016/j.gtc.2014.11.002
Mayor Barrera V, Aponte Martin DM, Prieto Ortíz RG, Orjuela Quiroga JE. Diagnóstico y tratamiento actual de la gastroparesia: una revisión sistemática de la literatura. Rev Colomb Gastroenterol. 2020;35(4):471-84. https://doi.org/10.22516/25007440.561
Hasler WL. Gastroparesis: pathogenesis, diagnosis and management. Nat Rev Gastroenterol Hepatol. 2011;8(8):438-53. https://doi.org/10.1038/nrgastro.2011.116
Ye Y, Jiang B, Manne S, Moses PL, Almansa C, Bennett D, et al. Epidemiology and outcomes of gastroparesis, as documented in general practice records, in the United Kingdom. Gut. 2021;70(4):644-53. https://doi.org/10.1136/gutjnl-2020-321277
Syed AR, Wolfe MM, Calles-Escandon J. Epidemiology and Diagnosis of Gastroparesis in the United States: A Population-based Study. J Clin Gastroenterol. 2020;54(1):50-4. https://doi.org/10.1097/MCG.0000000000001231
Maia Bosca M, Martí L, Mínguez M. Aproximación diagnóstica y terapéutica al paciente con gastroparesia. Gastroenterol Hepatol. 2007;30(6):351-9. https://doi.org/10.1157/13107570
Horowitz M, Su YC, Rayner CK, Jones KL. Gastroparesis: Prevalence, Clinical Significance and Treatment. Can J Gastroenterol. 2001;15(12):805-13. https://doi.org/10.1155/2001/628102
Farrell MB. Gastric Emptying Scintigraphy. J Nucl Med Technol. 2019;47(2):111-9. https://doi.org/10.2967/jnmt.117.227892
Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, et al. Consensus Recommendations for Gastric Emptying Scintigraphy: A Joint Report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008;36(1):44-54. https://doi.org/10.2967/jnmt.107.048116
Chaudhuri TK. Use of 99mTc-DTPA for measuring gastric emptying time. J Nucl Med. 1974;15(6):391-5.
Tamaş S, Dumitraşcu DL, Andreica V, Cotul S. Gastric sequential scintigraphy. Methodology with liquid isotonic meal. Physiologie. 1988;25(1-2):47-51.
Anvari M, Horowitz M, Fraser R, Maddox A, Myers J, Dent J, et al. Effects of posture on gastric emptying of nonnutrient liquids and antropyloroduodenal motility. Am J Physiol-Gastrointest Liver Physiol. 1995;268(5):G868-71. https://doi.org/10.1152/ajpgi.1995.268.5.G868
Farrell MB. Gastric Emptying Study: Liquids. J Nucl Med Technol. 2024;52(1):46-7. https://doi.org/10.2967/jnmt.124.267414
Ziessman HA, Okolo PI, Mullin GE, Chander A. Liquid gastric emptying is often abnormal when solid emptying is normal. J Clin Gastroenterol. 2009;43(7):639-43. https://doi.org/10.1097/MCG.0b013e318181b42f
Schol J, Wauters L, Dickman R, Drug V, Mulak A, Serra J, et al. United European Gastroenterology (UEG) and European Society for Neurogastroenterology and Motility (ESNM) consensus on gastroparesis. United Eur Gastroenterol J. 2021;9(3):287-306. https://doi.org/10.1002/ueg2.12060
Camilleri M, Kuo B, Nguyen L, Vaughn VM, Petrey J, Greer K, et al. ACG Clinical Guideline: Gastroparesis. Am J Gastroenterol. 2022;117(8):1197-220. https://doi.org/10.14309/ajg.0000000000001874
Sachdeva P, Malhotra N, Pathikonda M, Khayyam U, Fisher RS, Maurer AH, et al. Gastric Emptying of Solids and Liquids for Evaluation for Gastroparesis. Dig Dis Sci. 2011;56(4):1138-46. https://doi.org/10.1007/s10620-011-1635-9
Ziessman HA, Chander A, Clarke JO, Ramos AL, Wahl R. The Added Diagnostic Value of Liquid Gastric Emptying Compared with Solid Emptying Alone. J Nucl Med. 2009;50(5):726-31. https://doi.org/10.2967/jnumed.108.059790
Gentleman R, Ihaka R. R: The R Project for Statistical Computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2018.Disponible en: https://www.R-project.org/
Dean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, et al. Epi InfoTM, a database and statistics program for public health professionals. Atlanta, GA, USA: CDC; 2011.
Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(1):159-74. https://doi.org/10.2307/2529310
Barranco Castro D, del Pino Bellido P, Gómez Rodríguez B. Gastroparesis: diagnostic and therapeutic advances. Rev Andal Patol Dig. 2021;44(2):43-52. https://doi.org/10.37352/2021442.1
Lorena SLS, Tinois E, Hirata ES, Cunha ML, Brunetto SQ, Camargo EE, et al. Estudo do esvaziamento gástrico e da distribuição intragástrica de uma dieta sólida através da cintilografia: diferenças entre os sexos. Arq Gastroenterol. 2000;37(2):102-6. https://doi.org/10.1590/S0004-28032000000200006
Costa Barney V, Jaramillo Parra P, Luna Meza Á. Gastroparesia diabética: revisión corta con viñeta clínica ilustrativa. Actualización y puntos más relevantes para la práctica clínica. Rev Colomb Endocrinol Diabetes Metab. 2021;7(4):266-72. https://doi.org/10.53853/encr.7.4.653
Camilleri M, Sanders KM. Gastroparesis. Gastroenterology. 2022;162(1):68-87.e1.
https://doi.org/10.1053/j.gastro.2021.10.028.
Wang XJ, Burton DD, Breen-Lyles M, Camilleri M. Gastric accommodation influences proximal gastric and total gastric emptying in concurrent measurements conducted in healthy volunteers. Am J Physiol-Gastrointest Liver Physiol. 2021;320(5):G759-67. https://doi.org/10.1152/ajpgi.00008.2021
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















