Severe Hypocalcemia as an Atypical Manifestation of Seronegative Celiac Disease in a Patient with Systemic Lupus Erythematosus: Case Report
DOI:
https://doi.org/10.22516/25007440.971Keywords:
Celiac disease, lupus erythematosus systemic, Systemic lupus erythematosus, Hypocalcemia, Diarrhea, TetanyAbstract
Aim: To describe the clinical picture and diagnosis of an episode of severe hypocalcemia in a patient with systemic lupus erythematosus (SLE) in remission, with chronic diarrhea that led to the diagnosis of celiac disease (CD).
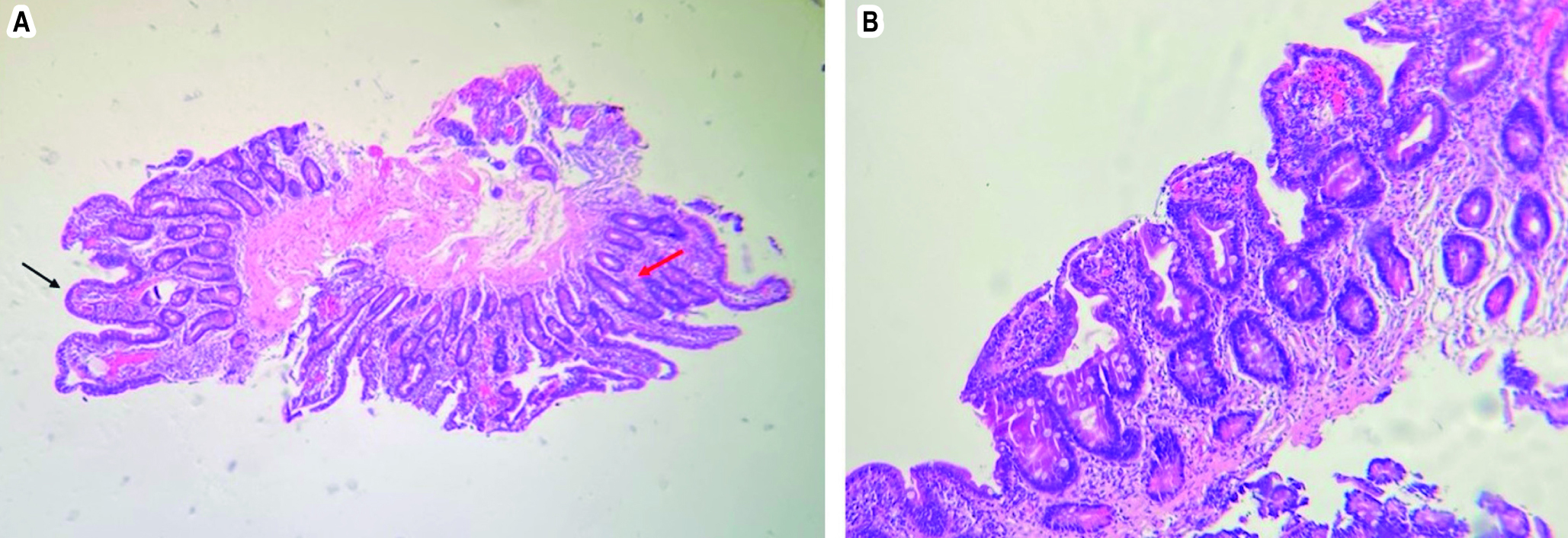
Case presentation: 22-year-old patient, diagnosed with SLE at age 10, in remission. He consulted for a two-month history of paresthesias, muscle spasms, myalgias, and episodes of tetany in the previous week, associated with malabsorptive postprandial diarrhea. His laboratory tests showed severe hypocalcemia, vitamin D deficiency, severe hypomagnesemia, and mild hypokalemia. In the study for CD, serology reported normal anti-tissue transglutaminase IgA, antigliadin IgA, and IgG and low total IgA levels. Enteroscopy revealed erosive bulbo-duodenitis, with villous atrophy and increased intraepithelial lymphocytes in the pathology, which, together with the immunohistochemical study, allowed the diagnosis of CD, Marsh 3a type. Management was initiated with a gluten-free diet, with a positive clinical response.
Conclusion: CD should be suspected in patients with SLE who present with diarrhea, abdominal pain, nausea/vomiting, recurrent oral aphthosis, and anemia. In rare seronegative CD cases, other causes of villous atrophy, mainly infectious, toxic, and immunological, must be ruled out. There is an association between CD and SLE, so diagnosis must be early and timely with the best testing scheme available to achieve effective treatment before complications occur.
Downloads
References
King JA, Jeong J, Underwood FE, Quan J, Panaccione N, Windsor JW, et al. Incidence of Celiac Disease Is Increasing Over Time: A Systematic Review and Meta-analysis. Am J Gastroenterol. 2020;115(4):507-25. https://doi.org/10.14309/ajg.0000000000000523
Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, Catassi C, et al. Celiac disease: a comprehensive current review. BMC Med. 2019;17(1):1-20. https://doi.org/10.1186/s12916-019-1380-z
Rubin JE, Crowe SE. Celiac disease. Ann Intern Med. 2020;172(1):ITC1-16. https://doi.org/10.7326/AITC202001070
Dahan S, Shor DBA, Comaneshter D, Tekes-Manova D, Shovman O, Amital H, et al. All disease begins in the gut: Celiac disease co-existence with SLE. Autoimmun Rev. 2016;15(8):848-53. https://doi.org/10.1016/j.autrev.2016.06.003
Courtney PA, Patterson RN, Lee RJE, McMillan SA. Systemic lupus erythematosus and coeliac disease. Lupus. 2004;13(3):214. https://doi.org/10.1191/0961203304lu512xx
Ebert EC, Hagspiel KD. Gastrointestinal and hepatic manifestations of systemic lupus erythematosus. J Clin Gastroenterol. 2011;45(5):436-41. https://doi.org/10.1097/MCG.0b013e31820f81b8
Tian XP, Zhang X. Gastrointestinal involvement in systemic lupus erythematosus: insight into pathogenesis, diagnosis and treatment. World J Gastroenterol. 2010;16(24):2971-7. https://doi.org/10.3748/wjg.v16.i24.2971
Mooney PD, Hadjivassiliou M, Sanders DS. Coeliac disease. BMJ. 2014;348:g1561. https://doi.org/10.1136/bmj.g1561
Ross JR, Gibb SP, Hoffman DE, Clerkin EP, Dotter WE, Hurxthal LM. Gluten Enteropathy and Skeletal Disease. JAMA. 1966;196(3):270-4. https://doi.org/10.1001/jama.1966.03100160120035
Staun M, Jarnum S. Measurement of the 10,000-molecular weight calcium-binding protein in small-intestinal biopsy specimens from patients with malabsorption syndromes. Scand J Gastroenterol. 1988;23(7):827-32. https://doi.org/10.3109/00365528809090768
Aziz I, Peerally MF, Barnes JH, Kandasamy V, Whiteley JC, Partridge D, et al. The clinical and phenotypical assessment of seronegative villous atrophy; a prospective UK centre experience evaluating 200 adult cases over a 15-year period (2000-2015). Gut. 2017;66(9):1563-72. https://doi.org/10.1136/gutjnl-2016-312271
Volta U, Caio G, Boschetti E, Giancola F, Rhoden KJ, Ruggeri E, et al. Seronegative celiac disease: shedding light on an obscure clinical entity. Dig Liver Dis. 2017;48(9):1018-22. https://doi.org/10.1016/j.dld.2016.05.024
Rensch MJ, Szyjkowski R, Shaffer RT, Fink S, Kopecky C, Grissmer L, et al. The prevalence of celiac disease autoantibodies in patients with systemic lupus erythematosus. Am J Gastroenterol. 2001;96(4):1113-5. https://doi.org/10.1111/j.1572-0241.2001.03753.x
Soltani Z, Baghdadi A, Nejadhosseinian M, Faezi ST, Shahbazkhani B, Mousavi SA, et al. Celiac disease in patients with systemic lupus erythematosus. Reumatologia. 2021;59(2):85-9. https://doi.org/10.5114/reum.2021.105416
Zitouni M, Daoud W, Kallel M, Makni S. Association entre lupus érythémateux systémique et maladie coeliaque: cinq cas. Revue du rhumatisme. 2004;71(7):630-32. https://doi.org/10.1016/S1169-8330(03)00392-2
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















