Intestinal Nonrotation, Imaging Findings in the Malrotation Spectrum: Case Report
DOI:
https://doi.org/10.22516/25007440.967Keywords:
Diagnostic imaging, Volvulus, congenital abnormalitiesAbstract
Intestinal nonrotation is a rare embryonic developmental anomaly with a reported incidence of up to 0.5% in autopsies. Given the asymptomatic course, the diagnosis may be late, so it becomes an incidental finding. This study presents the most common imaging characteristics to familiarize readers with this pathology.
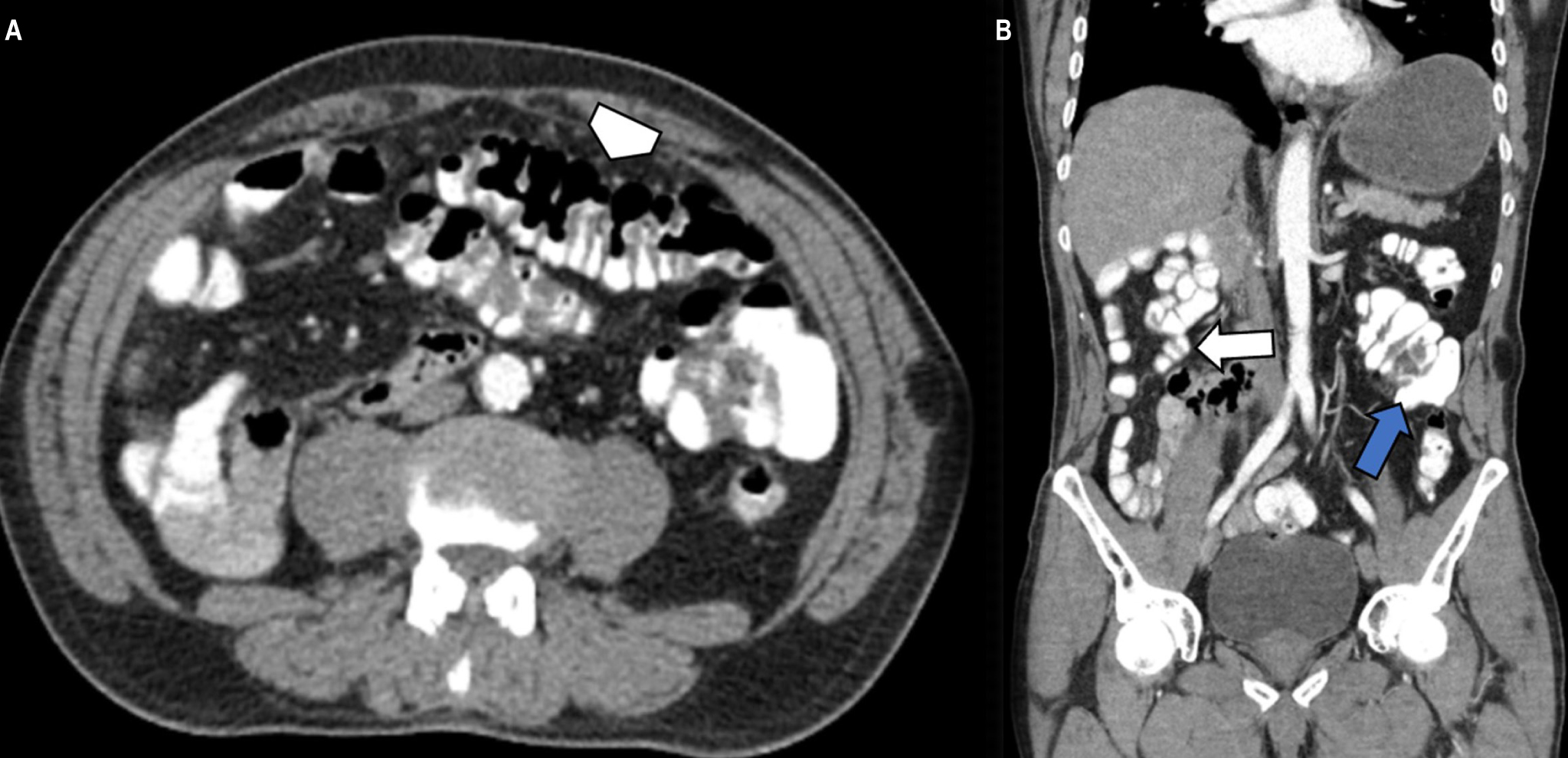
We describe the case of a 73-year-old patient who consulted for pain in the right inguinal region associated with the sensation of a mass. There were no significant findings on physical examination. An abdominal tomography with contrast was requested as a study method, identifying a reversal of the superior mesenteric artery/superior mesenteric vein relationship with the cecum, appendix, and ileocecal valve in the left flank and mesogastrium. A displacement of thin intestinal loops towards the right hemiabdomen was also noted.
Downloads
References
Choi M, Borenstein SH, Hornberger L, Langer JC. Heterotaxia syndrome: the role of screening for intestinal rotation abnormalities. Arch Dis Child. 2005;90(8):813-5. https://doi.org/10.1136/adc.2004.067504
Langer JC. Intestinal Rotation Abnormalities and Midgut Volvulus. Surg Clin North Am. 2017;97(1):147-59. https://doi.org/10.1016/j.suc.2016.08.011
Sözen S, Güzel K. Intestinal malrotation in an adult: case report. Ulus Travma Acil Cerrahi Derg. 2012;18(3):280-2. https://doi.org/10.5505/tjtes.2012.60973
Appaji AC, Kulkarni R, Kadaba JS. Nonrotation of intestine: a case report. J Clin Diagn Res. 2013;7(11):2575-6. https://doi.org/10.7860/JCDR/2013/6177.3616
Mohan P, Ramamoorthy M, Venkataraman J. Clinical vistas: nonrotation of the intestine. CMAJ. 2008 Jul 1;179(1):49-50. https://doi.org/10.1503/cmaj.080038
Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26(5):1485-500. https://doi.org/10.1148/rg.265055167
Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery. 201;149(3):386-93. https://doi.org/10.1016/j.surg.2010.07.004
Xiong Z, Shen Y, Morelli JN, Li Z, Hu X, Hu D. CT facilitates improved diagnosis of adult intestinal malrotation: a 7-year retrospective study based on 332 cases. Insights Imaging. 2021;12(1):58. https://doi.org/10.1186/s13244-021-00999-3
Diaz M, Reichard K, Taylor A. Intestinal nonrotation in an adolescent. Pediatr Emerg Care. 2009;25(4):249-51. https://doi.org/10.1097/PEC.0b013e31819e36aa
Gohl ML, DeMeester TR. Midgut nonrotation in adults. An aggressive approach. Am J Surg. 1975;129(3):319-23. https://doi.org/10.1016/0002-9610(75)90249-4
Strouse PJ. Disorders of intestinal rotation and fixation “malrotation”. Pediatr Radiol. 2004;34(11):837-51. https://doi.org/10.1007/s00247-004-1279-4
Gandhi V, Pai N, Kashiva R, Mane D. Adult with intestinal malrotation and colocolic intussusception: an unusual combo. BMJ Case Rep. 2019;12(7):e226398. https://doi.org/10.1136/bcr-2018-226398
Pourmand A, Dimbil U, Drake A, Shokoohi H. The Accuracy of Point-of-Care Ultrasound in Detecting Small Bowel Obstruction in Emergency Department. Emerg Med Int. 2018;2018:3684081. https://doi.org/10.1155/2018/3684081
Kapfer SA, Rappold JF. Intestinal malrotation-not just the pediatric surgeon’s problem. J Am Coll Surg. 2004;199(4):628-35. https://doi.org/10.1016/j.jamcollsurg.2004.04.024
Vandendries C, Jullès MC, Boulay-Coletta I, Loriau J, Zins M. Diagnosis of colonic volvulus: findings on multidetector CT with three-dimensional reconstructions. Br J Radiol. 2010;83(995):983-90. https://doi.org/10.1259/bjr/35714052
Etchevers J, Palermo M, Salvatore M, Tarsitano F,Villafañe V. Malrotación intestinal en adultos: causa infrecuente de abdomen agudo oclusivo. Rev Argentina de Radiol. 2008;72(4):435-38.
Tummala P, Junaidi O, Agarwal B. Imaging of pancreatic cancer: An overview. J Gastrointest Oncol. 2011;2(3):168-74. https://doi.org/10.3978/j.issn.2078-6891.2011.036
Chandra J, Grierson C, Bungay H. Normal variations in pancreatic contour are associated with intestinal malrotation and can mimic neoplasm. Clin Radiol. 2012;67(12):1187-92. https://doi.org/10.1016/j.crad.2011.11.021
Zissin R, Rathaus V, Oscadchy A, Kots E, Gayer G, Shapiro-Feinberg M. Intestinal malrotation as an incidental finding on CT in adults. Abdom Imaging. 1999;24(6):550-5. https://doi.org/10.1007/s002619900560
Pagkratis S, Kryeziu S, Lin M, Hoque S, Bucobo JC, Buscaglia JM, et al. Case report of intestinal non-rotation, heterotaxy, and polysplenia in a patient with pancreatic cancer. Medicine (Baltimore). 2017;96(49):e8599. https://doi.org/10.1097/MD.0000000000008599
Brungardt JG, Liebscher SC, Schropp KP. Malrotation Correction in the Adult Population. World J Surg. 2021;45(1):141-47. https://doi.org/10.1007/s00268-020-05790-x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















