Morphological Characteristics of the Duodenal Papilla and its Association with Complications Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) in a Peruvian Hospital
DOI:
https://doi.org/10.22516/25007440.859Keywords:
Endoscopic retrograde cholangiopancreatography, Ampulla of Vater, Adverse effects, EndoscopyAbstract
Introduction: several risk factors exist for complications post-endoscopic retrograde cholangiopancreatography (ERCP), and the morphology of the duodenal papilla is among those recently studied.
Objectives: to evaluate the association between the morphological characteristics of the duodenal papilla and post-ERCP complications in patients seen in the gastroenterology unit of a Peruvian referral hospital.
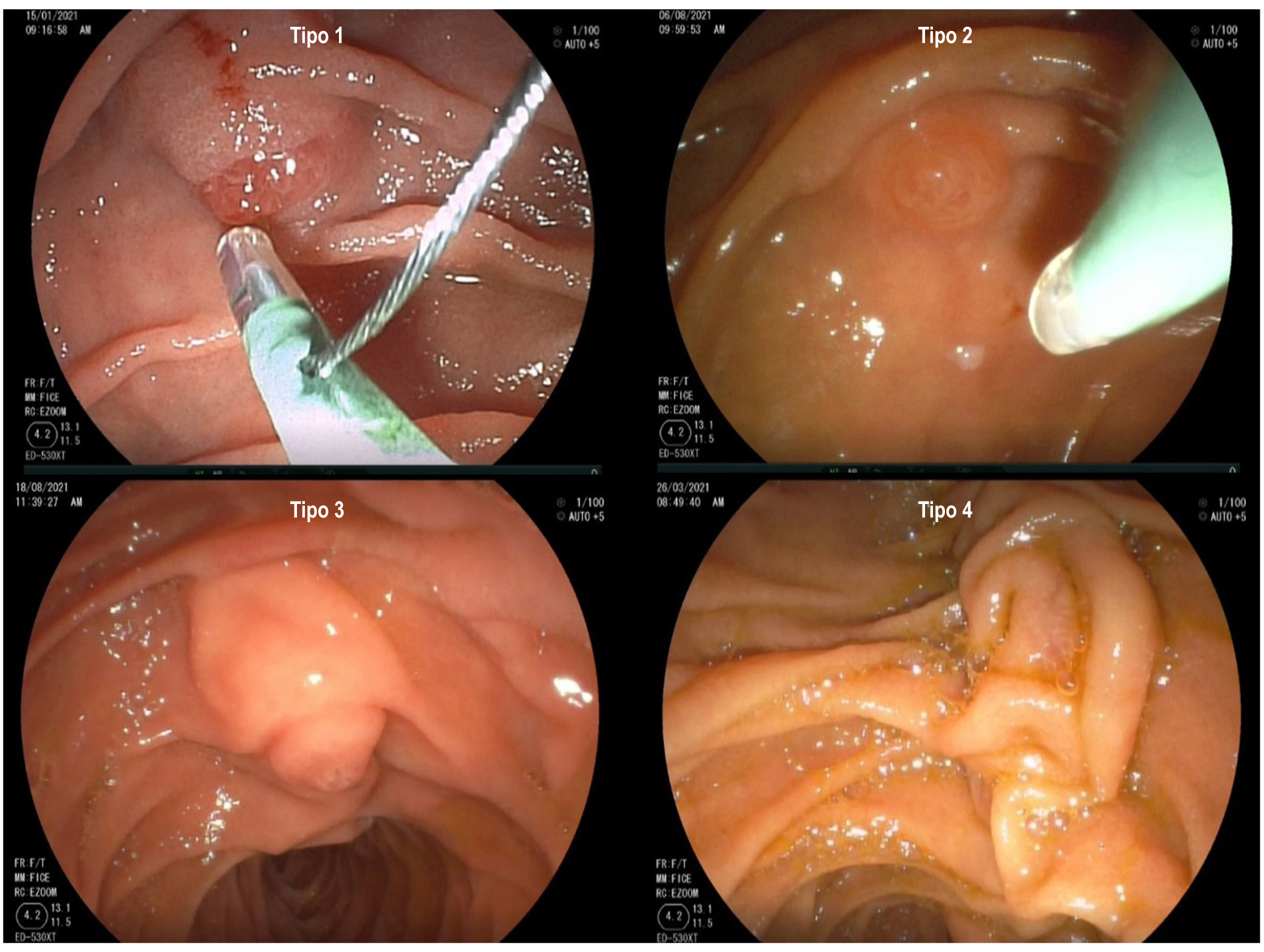
Methods: a prospective and analytical study including 138 patients who underwent ERCP, establishing a relationship between the type of duodenal papilla according to the endoscopic classification proposed by Haraldsson et al. and post-ERCP complications for up to 1 month of follow-up.
Results: one hundred thirty-eight patients were included, 93 were females (68.42%), and 45 were males (31.58%), with 51.46 years of mean age. Type 1 was associated with less difficulty in cannulation, with an odds ratio (OR): 0.42 (confidence interval [CI]: 0.20–0.88). Type 4 had a significantly longer cannulation time (6.83 minutes). The post-ERCP ratio for pancreatitis was 2.9%; bleeding, 1.45%, and perforation, 0.72%. The perforation showed a statistically significant association with papilla type (p = 0.009). Type 2 showed higher rates of pancreatitis (9.09%) and post-ERCP perforation (9.09%).
Conclusion: the duodenal papilla type is significantly associated with post-ERCP perforation. Type 2 showed higher complication rates.
Downloads
References
McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6. https://doi.org/10.1097/00000658-196805000-00013
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointestinal Endosc. 1974;20(4):148-51. https://doi.org/10.1016/s0016-5107(74)73914-1
Classen M, Demling L. Endoskopische sphinkterotomie der papila vateri und steinextrakion aus dem ductus choledochus. Dtsch Med Wochenschr. 1974;99(11):496-7. https://doi.org/10.1055/s-0028-1107790.
Dumonceau JM, Capral C, Aabakken L. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2020;52(2):127-149. https://doi.org/10.1055/a-1075-4080
Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. 2010;42(5):381-8. https://doi.org/10.1055/s-0029-1243992
Horiuchi A, Nakayama Y, Kajiyama M, Tanaka N. Effect of precut sphincterotomy on biliary cannulation based on the characteristics of the major duodenal papilla. Clin Gastroenterol Hepatol. 2007;5(9):1113-8. https://doi.org/10.1016/j.cgh.2007.05.014
Canena J, Lopes L, Fernandes J, Costa P, Arvanitakis M, Koch AD, et al. Influence of a novel classification of the papilla of Vater on the outcome of needle-knife fistulotomy for biliary cannulation. BMC Gastroenterol. 2021;21(1):147. https://doi.org/10.1186/s12876-021-01735-3
Haraldsson E, Lundell L, Swahn F, Enochsson L, Löhr J, Arnelo U. Endoscopic classification of the papilla of Vater. Results of an inter- and intraobserver agreement study. United Eur Gastroenterol J. 2017;5(4):504-10. https://doi.org/10.1177/2050640616674837
Haraldsson E, Kylänpää L, Grönroos J, Saarela A, Toth E, Qvigstad G, et al. The macroscopic appearance of the major duodenal papilla influences bile duct cannulation: a prospective multicenter study by the Scandinavian Association for Digestive Endoscopy study group for ERCP. Gastrointest Endosc. 2019;90(6):957-963. https://doi.org/10.1016/j.gie.2019.07.014
Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2016;48(7):657-83. https://doi.org/10.1055/s-0042-108641
Watanabe M, Okuwaki K, Kida M, Imaizumi H, Yamauchi H, Kaneko T, et al. Transpapillary Biliary Cannulation is Difficult in Cases with Large Oral Protrusion of the Duodenal Papilla. Dig Dis Sci. 2019;64(8):2291-2299. https://doi.org/10.1007/s10620-019-05510-z
Balan GG, Arya M, Catinean A, Sandru V, Moscalu M, Constantinescu G, et al. Anatomy of Major Duodenal Papilla Influences ERCP Outcomes and Complication Rates: A Single Center Prospective Study. J Clin Med. 2020;9(6):1637. https://doi.org/10.3390/jcm9061637
Chen PH, Tung CF, Peng YC, Yeh HZ, Chang CS, Chen CC. Duodenal major papilla morphology can affect biliary cannulation and complications during ERCP, an observational study. BMC Gastroenterol. 2020;20(1):310. https://doi.org/10.1186/s12876-020-01455-0
Mohamed R, Lethebe BC, Gonzalez-Moreno E, Kayal A, Bass S, Cole M, et al. Morphology of the major papilla predicts ERCP procedural outcomes and adverse events. Surg Endosc. 2021;35(12):6455-6465. https://doi.org/10.1007/s00464-020-08136-9
Zhang QS, Xu JH, Dong ZQ, Gao P, Shen YC. Success and Safety of Needle Knife Papillotomy and Fistulotomy Based on Papillary Anatomy: A Prospective Controlled Trial. Dig Dis Sci. 2022;67(5):1901-1909. https://doi.org/10.1007/s10620-021-06983-7
Wang X, Zhao J, Wang L, Ning B, Zeng W, Tao Q, et al. Relationship between papilla-related variables and post endoscopic retrograde cholangiopancreatography pancreatitis: A multicenter, prospective study. J Gastroenterol Hepatol. 2020;35(12):2184-2191. https://doi.org/10.1111/jgh.15135
Adler DG. ERCP biliary cannulation difficulty as a function of papillary subtypes: a tale of shapes and Shar-Pei dogs. Gastrointest Endosc. 2019;90(6):964-965. https://doi.org/10.1016/j.gie.2019.07.030
Katsinelos P, Gkagkalis S, Chatzimavroudis G, Beltsis A, Terzoudis S, Zavos C, et al. Comparison of three types of precut technique to achieve common bile duct cannulation: a retrospective analysis of 274 cases. Dig Dis Sci. 2012;57(12):3286-92. https://doi.org/10.1007/s10620-012-2271-8
Hew S, Bechara R, Hookey L. Papillary morphology influences biliary cannulation: beware the small papilla. Gastrointest Endosc. 2020;91(4):959. https://doi.org/10.1016/j.gie.2019.12.005
Zuber-Jerger I, Gelbmann MC, Kullmann F. Visual characteristics of the papilla to estimate cannulation of the common bile duct - a pilot study. N Am J Med Sci. 2009;1(2):66-73.
Han S, Baek D, Kim D, Park Ch, Park Y, Lee M, et al. Primary needle-knife fistulotomy for preventing post-endoscopic retrograde cholangiopancreatography pancreatitis: Importance of the endoscopist’s expertise level. World J Clin Cases. 2021;9(17):4166-4177. https://doi.org/10.12998/wjcc.v9.i17.4166
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















