Microscopic colitis: Case series and literature review
DOI:
https://doi.org/10.22516/25007440.817Keywords:
diarrhea, microscopic colitis, lymphocytic, collagen, budesonideAbstract
Introduction: Microscopic colitis is a benign and multifactorial disease characterized by watery diarrhea and histological alterations in the colonic mucosa. The incidence of this disease is increasing, being diagnosed more frequently.
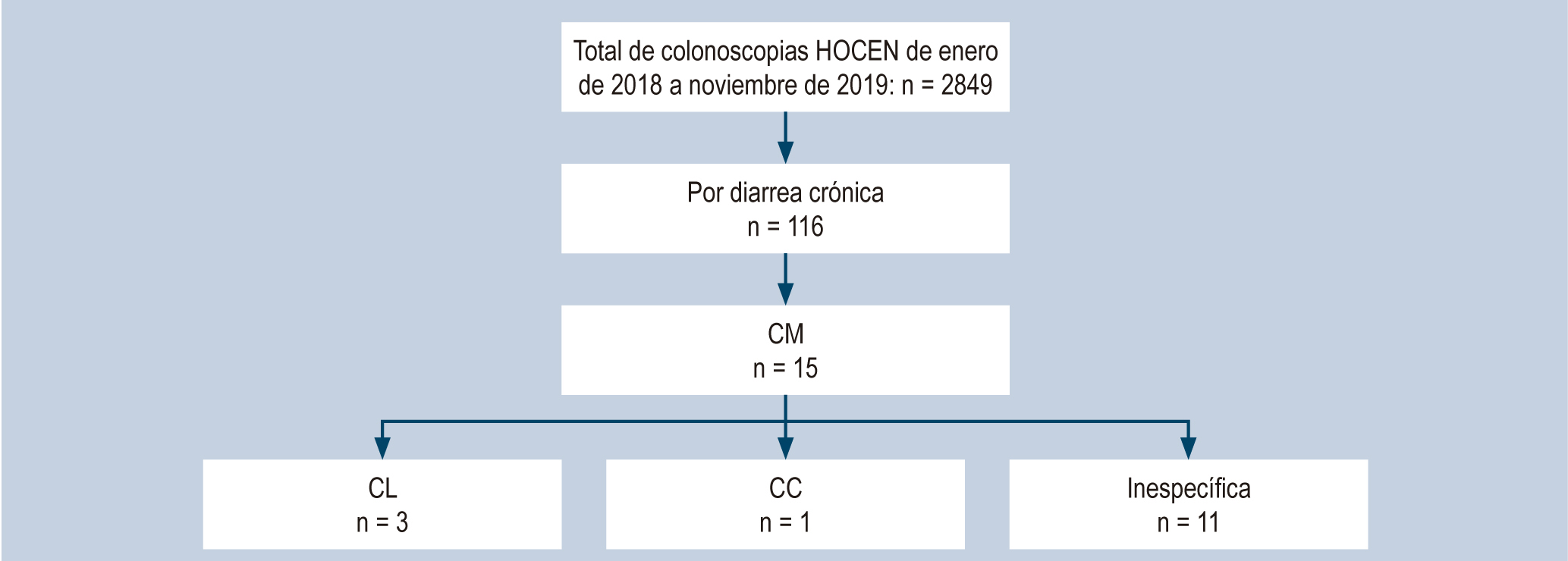
Materials and methods: In this retrospective study, patients were examined employing colonoscopy and biopsy due to a diagnosis of chronic diarrhea in a gastroenterology unit throughout 22 months. Their diagnosis of colitis was confirmed by clinical picture and microscopic analysis.
Results: In the study period, a total of 2849 colonoscopies were performed, 116 in patients with chronic diarrhea. We identified 15 patients with microscopic colitis, 12 were men (80 %), and only three were older than 60 (20 %).
Conclusion: Unlike the world literature, this study found that microscopic colitis in our patients affects the male sex primarily (male/female ratio: 4/1) and occurs in young people, with an average age of 47.5 years (range: 21–82 years).
Downloads
References
Miehlke S, Verhaegh B, Tontini GE, Madisch A, Langner C, Münch A. Microscopic colitis: pathophysiology and clinical management. Lancet Gastroenterol Hepatol. 2019;4(4):305-314. https://doi.org/10.1016/S2468-1253(19)30048-2
Pardi DS. Diagnosis and Management of Microscopic Colitis. Am J Gastroenterol. 2017;112(1):78-85. https://doi.org/10.1038/ajg.2016.477
Carrasco-Labra A, Lytvyn L, Falck-Ytter Y, Surawicz CM, Chey WD. AGA Technical Review on the Evaluation of Functional Diarrhea and Diarrhea-Predominant Irritable Bowel Syndrome in Adults (IBS-D). Gastroenterology. 2019;157(3):859-880. https://doi.org/10.1053/j.gastro.2019.06.014
Hempel KA, Sharma AV. Collagenous And Lymphocytic Colitis. 2021. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
Tulassay Z, Mihaly E, Herszényi L. Microscopic Colitis: A Challenging Disorder. Dig Dis. 2020;38(2):117-121. https://doi.org/10.1159/000505263
Bielsa-Fernández MV. Enteritis y colitis microscópicas. Rev Gastroenterol México. 2017;82(Supl 1):85-87.
Prieto-Ortíz RG, Prieto-Ortíz JE. Colitis microscópica, un diagnóstico en aumento. Rev Colomb Gastroenterol. 2019;34(4):399-403. https://doi.org/10.22516/25007440.377
Bauta J, Pupo A. Colitis microscópica. Correo Científico Médico. 2017;21(2):526-539.
Rojas R. Diagnóstico y manejo de la colitis microscópica. Gastroenterol Latinoam. 2019;30(Supl 1):S35-S38.
Solberg F, Ohlsson B. Microscopic colitis and its associations with complications observed in classic inflammatory bowel disease: a systematic review. Scand J Gastroenterol. 2020;55(3):312-320. https://doi.org/10.1080/00365521.2020.1739325
Tong J, Zheng Q, Zhang C, Lo R, Shen J, Ran Z. Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysis. Am J Gastroenterol. 2015;110(2):265-76; quiz 277. https://doi.org/10.1038/ajg.2014.431
Fernandez-Bañares F, Esteve M, Salas A, Forné TM, Espinos JC, Martín-Comin J, et al. Bile acid malabsorption in microscopic colitis and in previously unexplained functional chronic diarrhea. Dig Dis Sci. 2001;46(10):2231-8.
https://doi.org/10.1023/a:1011927302076
Jaruvongvanich V, Poonsombudlert K, Ungprasert P. Smoking and Risk of Microscopic Colitis: A Systematic Review and Meta-analysis. Inflamm Bowel Dis. 2019;25(4):672-678. https://doi.org/10.1093/ibd/izy296
Larsson JK, Sonestedt E, Ohlsson B, Manjer J, Sjöberg K. The association between the intake of specific dietary components and lifestyle factors and microscopic colitis. Eur J Clin Nutr. 2016;70(11):1309-1317. https://doi.org/10.1038/ejcn.2016.130.
Townsend T, Campbell F, O›Toole P, Probert C. Microscopic colitis: diagnosis and management. Frontline Gastroenterol. 2019;10(4):388-393. https://doi.org/10.1136/flgastro-2018-101040
Ingle SB, Adgaonkar BD, Ingle CR. Microscopic colitis: Common cause of unexplained nonbloody diarrhea. World J Gastrointest Pathophysiol. 2014;5(1):48-53. https://doi.org/10.4291/wjgp.v5.i1.48
Münch A, Sanders DS, Molloy-Bland M, Hungin APS. Undiagnosed microscopic colitis: a hidden cause of chronic diarrhoea and a frequently missed treatment opportunity. Frontline Gastroenterol. 2019;11(3):228-234.
https://doi.org/10.1136/flgastro-2019-101227
Cotter TG, Binder M, Loftus EV Jr, Abboud R, McNally MA, Smyrk TC, et al. Development of a Microscopic Colitis Disease Activity Index: a prospective cohort study. Gut. 2018;67(3):441-446. https://doi.org/10.1136/gutjnl-2016-313051
Shor J, Churrango G, Hosseini N, Marshall C. Management of microscopic colitis: challenges and solutions. Clin Exp Gastroenterol. 2019;12:111-120. https://doi.org/10.2147/CEG.S165047
Miehlke S, Acosta MB, Bouma G, Carpio D, Magro F, Moreels T, et al. Oral budesonide in gastrointestinal and liver disease: A practical guide for the clinician. J Gastroenterol Hepatol. 2018. https://doi.org/10.1111/jgh.14151
Baert F, Schmit A, D›Haens G, Dedeurwaerdere F, Louis E, Cabooter M, et al. Budesonide in collagenous colitis: a double-blind placebo-controlled trial with histologic follow-up. Gastroenterology. 2002;122(1):20-5. https://doi.org/10.1053/gast.2002.30295
Miehlke S, Madisch A, Kupcinskas L, Petrauskas D, Böhm G, Marks HJ, et al. Budesonide is more effective than mesalamine or placebo in short-term treatment of collagenous colitis. Gastroenterology. 2014;146(5):1222-30.e1-2. https://doi.org/10.1053/j.gastro.2014.01.019
Münch A, Bohr J, Miehlke S, Benoni C, Olesen M, Öst Å, et al. Low-dose budesonide for maintenance of clinical remission in collagenous colitis: a randomised, placebo-controlled, 12-month trial. Gut. 2016;65(1):47-56. https://doi.org/10.1136/gutjnl-2014-308363
Miehlke S, Aust D, Mihaly E, Armerding P, Böhm G, Bonderup O, et al. Efficacy and Safety of Budesonide, vs Mesalazine or Placebo, as Induction Therapy for Lymphocytic Colitis. Gastroenterology. 2018;155(6):1795-1804.e3. https://doi.org/10.1053/j.gastro.2018.08.042
Rojo E, Casanova MJ, Gisbert JP. Tratamiento de la colitis microscópica: papel de la budesonida y nuevas alternativas en pacientes refractarios. Rev Esp Enferm Dig. 2020;112(1):53-58. https://doi.org/10.17235/reed.2019.6655/2019
Nguyen GC, Smalley WE, Vege SS, Carrasco-Labra A; Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on the Medical Management of Microscopic Colitis. Gastroenterology. 2016;150(1):242-6; quiz e17-8. https://doi.org/10.1053/j.gastro.2015.11.008
Chande N, Al Yatama N, Bhanji T, Nguyen TM, McDonald JW, MacDonald JK. Interventions for treating lymphocytic colitis. Cochrane Database Syst Rev. 2017;7(7):CD006096. https://doi.org/10.1002/14651858.CD006096.pub4
Münch A, Söderholm JD, Wallon C, Ost A, Olaison G, Ström M. Dynamics of mucosal permeability and inflammation in collagenous colitis before, during, and after loop ileostomy. Gut. 2005;54(8):1126-8. https://doi.org/10.1136/gut.2004.058750
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















