Can We Use the Indication for a Colonoscopy as a Predictor of the Adenoma Detection Rate?
DOI:
https://doi.org/10.22516/25007440.743Keywords:
Colonoscopy, adenoma, surveillance, ScreeningAbstract
Aim: To determine the adenoma detection rate (ADR) and identify the indications for a colonoscopy that predict adenomas.
Materials and methods: Cross-sectional study. We included patients older than 18 years who underwent colonoscopy between February and July 2020 at a specialized center in Medellín, Colombia. We estimated the ADR and identified the indications for a colonoscopy, considered predictors for finding adenomas.
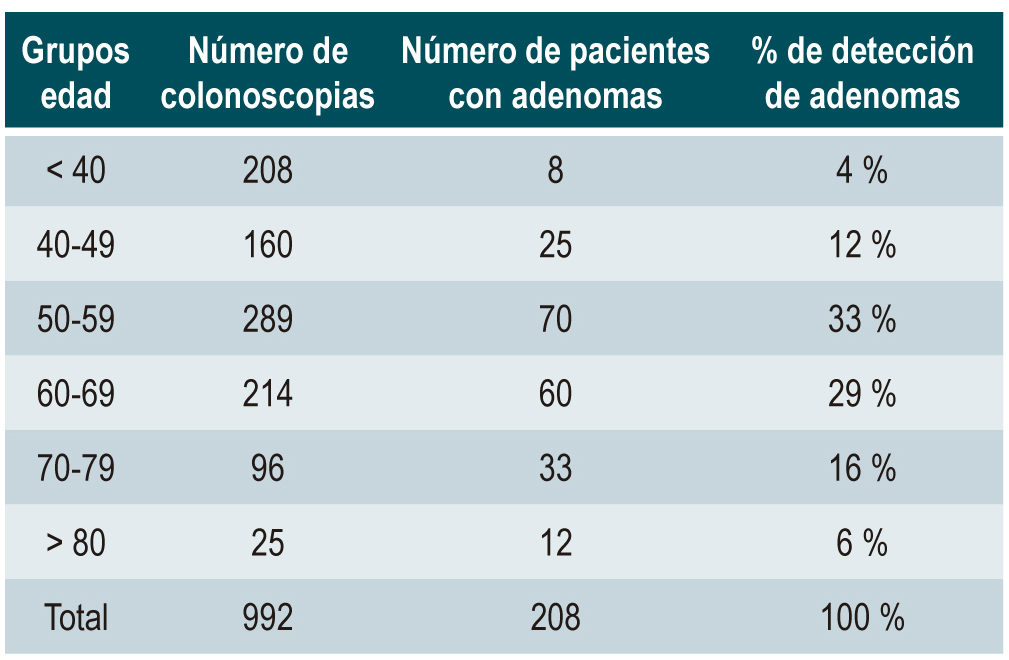
Results: The overall adenoma detection was 21 % (n = 992) and ADR in the screening population was 25 %. The range of 40-49 years contributed 12 % of the total number of adenomas detected, and the male population had a higher incidence (OR 1.73; 95 % CI 1.25-2.38; p < 0.001). Personal history of polyps (OR 1.86; 95 % CI 1.25-2.78; p = 0.002) and fecal occult blood (OR 2.67; 95 % CI 1.12-6.35; p 0.026) are deemed predictors for finding adenomas. LCI filters showed better results in detecting lesions (OR 1.43; 95 % CI 1.02-2.0).
Conclusions: The indications for a colonoscopy can predict the probability of detecting adenomas. Male gender, a personal history of polyps, fecal occult blood, and the search for adenomas after the age of 40 are the variables that increase the probability of finding adenomas. The use of LCI filters increases lesion detection. The suggested age to start CRC screening is 40 years.
Downloads
References
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370(14):1298-306. https://doi.org/10.1056/NEJMoa130908
Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, et al. quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010;362(19):1795-803. https://doi.org/10.1056/NEJMoa0907667
Ramírez-Quesada W, Vargas-Madrigal J, Alfaro-Murillo O, Umaña-Solís E, Campos-Goussen C, Alvarado-Salazar M, et al. Indicadores de calidad para la realización de colonoscopia. Acta Médica Costarric. 2019;61(1):37-42. https://doi.org/10.51481/amc.v61i1.1024
Schoenfeld P. Quality in colorectal cancer screening with colonoscopy. Gastrointest Endosc Clin N Am. 2020;30(3):541-51. https://doi.org/10.1016/j.giec.2020.02.014
Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366(8):687-96. https://doi.org/10.1056/NEJMoa1100370
Ladabaum U. Cost-effectiveness of current colorectal cancer screening tests. Gastrointest Endosc Clin N Am. 2020;30(3):479-97. https://doi.org/10.1016/j.giec.2020.02.005
Patel SG, Boland CR. Colorectal cancer in persons under age 50: Seeking causes and solutions. Gastrointest Endosc Clin N Am. 2020;30(3):441-55. https://doi.org/10.1016/j.giec.2020.03.001
Yang PF, Wong SW. Adenoma detection rate in colonoscopy: Is indication a predictor? Surg Laparosc Endosc Percutan Tech. 2016;26(2):156-61. https://doi.org/10.1097/SLE.0000000000000253
Millan MS, Gross P, Manilich E, Church JM. Adenoma detection rate: The real indicator of quality in colonoscopy. Dis Colon Rectum. 2008;51(8):1217-20. https://doi.org/10.1007/s10350-008-9315-3
Kaminski M, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees C, Dekker E, et al. Performance measures for lower gastrointestinal endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2017;49(4):378-97. https://doi.org/10.1055/s-0043-103411
Declaración de Helsinki de la AMM - Principios éticos para las investigaciones médicas en seres humanos [Internet]. Asociación Médica Mundial; 2013 (consultado el 12 de marzo de 2021). Disponible en: http://www.redsamid.net/archivos/201606/2013-declaracion-helsinki-brasil.pdf?1
Resolución número 8430 de 1993 [Internet]. Ministerio de Salud de Colombia; 1993 (consultado el 12 de marzo de 2021). Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.PDF
Sánchez del Río A, Pérez Romero S, López-Picazo J, Alberca de las Parras F, Júdez J, León Molina J. Indicadores de calidad en colonoscopia. Procedimiento de la colonoscopia. Rev Esp Enferm Dig. 2018;110(5):316-26. https://doi.org/10.17235/reed.2018.5408/2017
Azer SA. Challenges facing the detection of colonic polyps: What can deep learning do? Medicina (Kaunas). 2019 12;55(8):473. https://doi.org/10.3390/medicina55080473
Zhao S, Wang S, Pan P, Xia T, Chang X, Yang X, et al. Magnitude, risk factors, and factors associated with adenoma miss rate of tandem colonoscopy: A systematic review and meta-analysis. Gastroenterology. 2019;156(6):1661-74.e11. https://doi.org/10.1053/j.gastro.2019.01.260
Yamaguchi H, Fukuzawa M, Minami H, Ichimiya T, Takahashi H, Matsue Y, et al. The relationship between post-colonoscopy colorectal cancer and quality indicators of colonoscopy: The latest single-center cohort study with a review of the literature. Intern Med Tokyo Jpn. 2020;59(12):1481-8. https://doi.org/10.2169/internalmedicine.4212-19
Butterly LF. Proven strategies for increasing adherence to colorectal cancer screening. Gastrointest Endosc Clin N Am. 2020;30(3):377-92. https://doi.org/10.1016/j.giec.2020.02.003
Chen S, Sun K, Chao K, Sun Y, Hong L, Weng Z, et al. Detection rate and proximal shift tendency of adenomas and serrated polyps: A retrospective study of 62,560 colonoscopies. Int J Colorectal Dis. 2018;33(2):131-9. https://doi.org/10.1007/s00384-017-2951-0
Shaukat A, Holub J, Greenwald D, Eisen G, Schmitt C. Variation over time and factors associated with detection rates of sessile serrated lesion across the United States: Results form a national sample using the GIQuIC registry. Am J Gastroenterol. 2021;116(1):95-9. https://doi.org/10.14309/ajg.0000000000000824
Gil Parada FL, Torres Amaya M, Riveros Santoya SV, Castaño Llano R, Ibáñez H, Huertas Quintero MM, et al. Guía de práctica clínica para la tamización de cáncer colorrectal. Rev Colomb Gastroenterol. 2015;30(2):1-27.
Greenspan M, Rajan KB, Baig A, Beck T, Mobarhan S, Melson J. Advanced adenoma detection rate is independent of nonadvanced adenoma detection rate. Am J Gastroenterol. 2013;108(8):1286-92. https://doi.org/10.1038/ajg.2013.149
Butterly LF, Siegel RL, Fedewa S, Robinson CM, Jemal A, Anderson JC. Colonoscopy outcomes in average-risk screening equivalent young adults: Data from the New Hampshire colonoscopy registry. Am J Gastroenterol. 2021;116(1):171-9. https://doi.org/10.14309/ajg.0000000000000820
Klare P, Ascher S, Hapfelmeier A, Wolf P, Beitz A, Schmid RM, et al. Patient age and duration of colonoscopy are predictors for adenoma detection in both proximal and distal colon. World J Gastroenterol. 2015;21(2):525-32. https://doi.org/10.3748/wjg.v21.i2.525
Strum WB. Colorectal adenomas. N Engl J Med. 2016;374(11):1065-75. https://doi.org/10.1056/NEJMra1513581
Kolb JM, Ahnen DJ, Samadder NJ. Evidenced-based screening strategies for a positive family history. Gastrointest Endosc Clin N Am. 2020;30(3):597-609. https://doi.org/10.1016/j.giec.2020.02.015.
Kolb JM, Molmenti CL, Patel SG, Lieberman DA, Ahnen DJ. Increased risk of colorectal cancer tied to advanced colorectal polyps: An untapped opportunity to screen first-degree relatives and decrease cancer burden. Am J Gastroenterol. 2020;115(7):980-8. https://doi.org/10.14309/ajg.0000000000000639
van der Meulen-de Jong AE, Morreau H, Becx MCJM, Crobach LFSJ, van Haastert M, ten Hove WR, et al. High detection rate of adenomas in familial colorectal cancer. Gut. 2011;60(1):73-6. https://doi.org/10.1136/gut.2010.217091
Xiang L, Zhan Q, Wang XF, Zhao XH, Zhou YB, An SL, et al. Risk factors associated with the detection and missed diagnosis of colorectal flat adenoma: A Chinese multicenter observational study. Scand J Gastroenterol. 2018;53(12):1519-25. https://doi.org/10.1080/00365521.2018.1533581
Zamora Morales M, Zárate Guzmán ÁM, García Guerrero VA, Corral Medina A, Valdés Lias R. Determinación de tasa de adenomas desapercibidos en pacientes con riesgo promedio de cáncer colorrectal con preparación intestinal inadecuada. Endoscopia. 2016;28(2):49-54. https://doi.org/10.1016/j.endomx.2016.05.002
Sulz MC, Kröger A, Prakash M, Manser CN, Heinrich H, Misselwitz B. Meta-analysis of the effect of bowel preparation on adenoma detection: Early adenomas affected stronger than advanced adenomas. PloS One. 2016;11(6):e0154149. https://doi.org/10.1371/journal.pone.0154149
Han A, Maratt J, Kahi C. Colorectal cancer screening decisions in the opportunistic setting. Gastrointest Endosc Clin N Am. 2020;30(3):413-22. https://doi.org/10.1016/j.giec.2020.02.012
Robertson DJ, Selby K. Fecal immunochemical test: The world’s colorectal cancer screening test. Gastrointest Endosc Clin N Am. 2020;30(3):511-26. https://doi.org/10.1016/j.giec.2020.02.011
Kligman E, Li W, Eckert GJ, Kahi C. Adenoma detection rate in asymptomatic patients with positive fecal immunochemical tests. Dig Dis Sci. 2018;63(5):1167-72. https://doi.org/10.1007/s10620-018-4984-9
Herszényi L. The «difficult» colorectal polyps and adenomas: Practical aspects. Dig Dis Basel Switz. 2019;37(5):394-9. https://doi.org/10.1159/000495694
Núñez-Rodríguez H, Diez-Redondo P, Pérez-Miranda M, González Sagrado M, Conde R, De la Serna C. Role of full-spectrum endoscopy in colorectal cancer screening: Randomized trial. J Clin Gastroenterol. 2019;53(3):191-6. https://doi.org/10.1097/MCG.0000000000000975
Matsuda T, Ono A, Sekiguchi M, Fujii T, Saito Y. Advances in image enhancement in colonoscopy for detection of adenomas. Nat Rev Gastroenterol Hepatol. 2017;14(5):305-14. https://doi.org/10.1038/nrgastro.2017.18
Oliveira Dos Santos CE, Malaman D, Pereira-Lima JC, de Quadros Onófrio F, Ribas Filho JM. Impact of linked-color imaging on colorectal adenoma detection. Gastrointest Endosc. 2019;90(5):826-34. https://doi.org/10.1016/j.gie.2019.06.045
Yoshida N, Hisabe T, Ikematsu H, Ishihara H, Terasawa M, Inaba A, et al. Comparison between linked color imaging and blue laser imaging for improving the visibility of flat colorectal polyps: A multicenter pilot study. Dig Dis Sci. 2020;65(7):2054-62. https://doi.org/10.1007/s10620-019-05930-x
Wang P, Liu P, Glissen Brown JR, Berzin TM, Zhou G, Lei S, et al. Lower adenoma miss rate of computer-aided detection-assisted colonoscopy vs routine white-light colonoscopy in a prospective tandem study. Gastroenterology. 2020;159(4):1252-61.e5. https://doi.org/10.1053/j.gastro.2020.06.023
Cepeda Vásquez RA. Inteligencia artificial en la detección de pólipos colónicos: qué dicen los estudios. Rev Colomb Gastroenterol. 2021;36(1):2-6. https://doi.org/10.22516/25007440.726
Gómez Zuleta MA, Cano Rosales DF, Bravo Higuera DF, Ruano Balseca JA, Romero Castro E. Detección automática de pólipos colorrectales con técnicas de inteligencia artificial. Rev Colomb Gastroenterol. 2021;36(1):7-17. https://doi.org/10.22516/25007440.471
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















