Management of patients with inflammatory bowel disease during the COVID-19 pandemic
DOI:
https://doi.org/10.22516/25007440.537Keywords:
COVID-19, SARS-Cov-2, inflammatory bowel diseaseAbstract
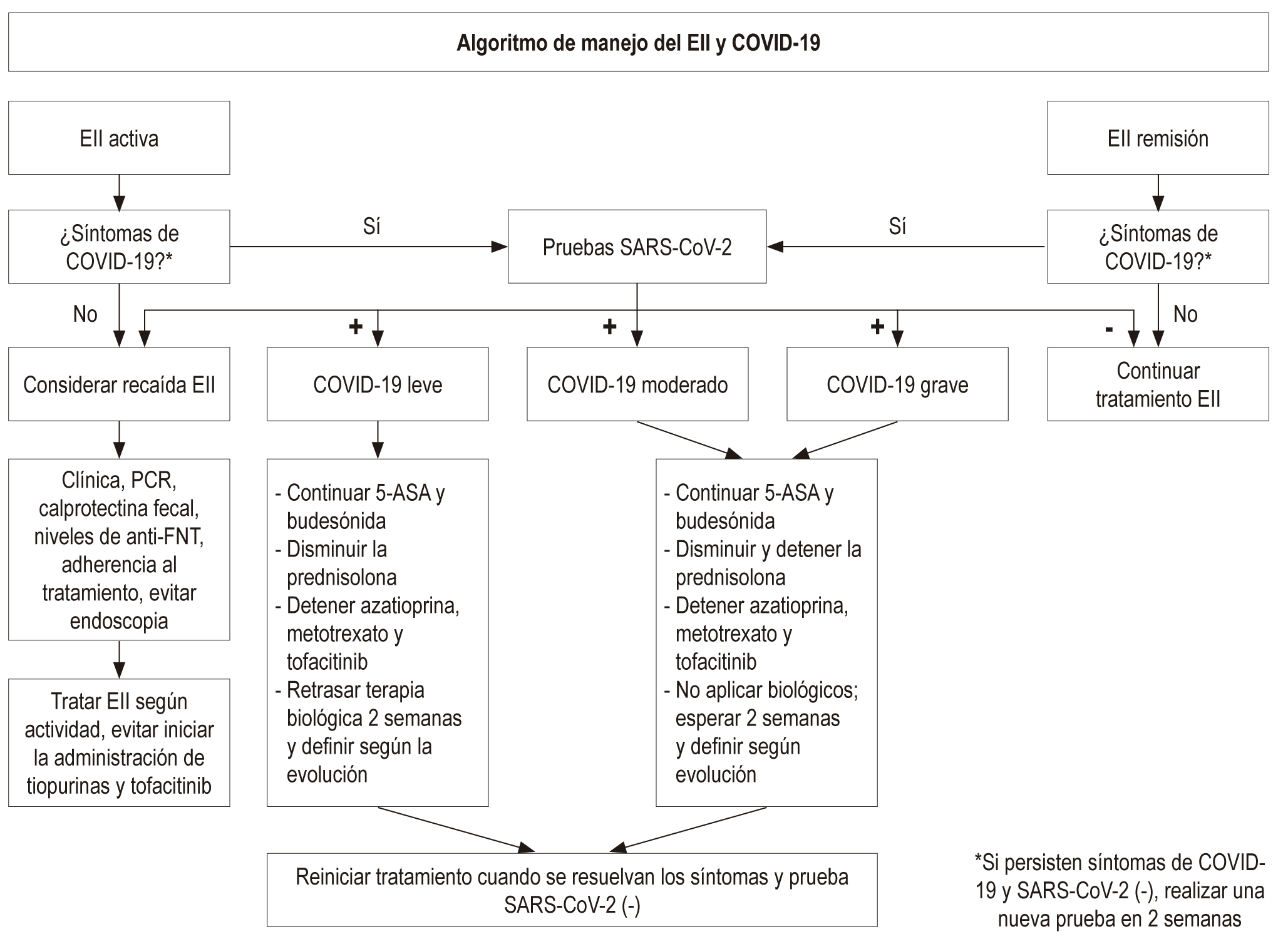
The pandemic caused by the SARS-Cov-2 virus originating in Wuhan, capital of the province of Hubei (China), has become a challenge for humanity. It is a highly contagious virus and up to now the COVID-19 disease has an overall mortality of around 6 %, which is higher in patients with comorbidities. Inflammatory bowel disease (IBD) is a disabling pathology, with tissue damage and impaired immune response, which, associated with immunosuppressive drugs that are frequently used for their treatment, put the patient at risk of developing infections and complications. In this review we consider the interaction of the SARS-CoV-2 virus with the gastrointestinal tract and the potential mechanisms whereby a patient with IBD could have an increased risk of COVID-19 infection. Additionally, and despite the fact that there are no published clinical studies in patients with IBD and COVID-19, we make recommendations based on the opinion of experts on the care of patients with IBD, with an emphasis on its treatment and the safe performance of endoscopic procedures, both for the patient and the health personnel.
Downloads
References
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implication for virus origins and receptor binding. Lancet 2020;395:565-574. https://doi.org/10.1016/S0140-6736(20)30251-8
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. https://doi.org/10.1056/NEJMoa2001017
World Health Organization [Internet]. Coronavirus. 2020 [acceso 15 de abril de 2020]. Disponible en: https://www.who.int/health-topics/coronavirus
Johns Hopkins University Coronavirus Resource Center [Internet]. Coronavirus COVID-19 Global Cases 2020 [acceso 15 de abril de 2020]. Disponible en: https://coronavirus.jhu.edu/map.html
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564-1567. https://doi.org/10.1056/NEJMc2004973
Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med. 2020; M20-0504. https://doi.org/10.1101/2020.02.02.20020016
Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARSCoV-2. Gastroenterology. 2020; S0016508520302821. https://doi.org/10.1053/j.gastro.2020.02.055
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. https://doi.org/10.1056/NEJMoa2001191
Borges do Nascimento IJ, Cacic N, Abdulazeem HM, Caspar von Groote T, Jayarajah U, Weerasekara I, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):E941. https://doi.org/10.3390/jcm9040941
Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648
Cheung KS, Hung I, Chang P, Lung KC, Tso E, Liu R, et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples from the Hong Kong Cohort and Systematic Review and Meta-analysis. 2020. https://doi.org/10.1053/j.gastro.2020.03.065
Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel J-F. Ulcerative Colitis. Lancet. 2017;389(10080):1756-1770. https://doi.org/10.1016/S0140-6736(16)32126-2
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn´s Disease. Lancet. 2017;389(10080):1741-1755. https://doi.org/10.1016/S0140-6736(16)31711-1
Ng SC, Shi HY, Hamidi N, Underwood FE, Whitney Tang W, Benchimol EL, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390(10114):2769-2778. https://doi.org/10.1016/S0140-6736(17)32448-0
Kotze PG, Underwood F, Damiao AOMC, Ferraz JG, Saad-Hossne R, Toro M, et al. Progression of Inflammatory Bowel Diseases Throughout Latin America and the Caribbean: A Systematic Review. Clin Gastroenterol Hepatol. 2020;18(2):304-312. https://doi.org/10.1016/j.cgh.2019.06.030
Bonovas S, Fiorino G, Allocca M, Lytras T, Nikolopoulos GK, Peyrin-Biroulet L, et al. Biologic Therapies and Risk of Infection and Malignancy in Patients with Inflammatory Bowel Disease: A Systematic Review and Network Meta-analysis. Clin Gastroenterol Hepatol. 2016;14(10):1385–1397. https://doi.org/10.1016/j.cgh.2016.04.039
Govani SM, Higgins PD. Combination of thiopurines and allopurinol: adverse events and clinical benefit in IBD. J Crohns Colitis. 2010;4(4):444–9. https://doi.org/10.1016/j.crohns.2010.02.009
Wisniewski A, Kirchgesner J, Seksik Ph, Landman C, Bourrier A, Nion-Larmurier I, et al. Increased incidence of systemic serious viral infections in patients with inflammatory bowel disease associates with active disease and use of thiopurines. United Eur. Gastroenterol. J. 2020;8(3):303-313. https://doi.org/10.1177/2050640619889763
Toruner M, Loftus EV, Harmsen WS, Zinsmeister AR, Orenstein R, Sandborn WJ, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology 2008;134(4):929–936. https://doi.org/10.1053/j.gastro.2008.01.012
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020. https://doi.org/10.1016/j.cell.2020.02.052
Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J Crohns Colitis. 2020. https://doi.org/10.1093/ecco-jcc/jjaa061
Garg M, Royce SG, Tikellis C, Shallue C, Batu D, Velkoska E, et al. Imbalance of the renin-angiotensin system may contribute to inflammation and fibrosis in IBD: a novel therapeutic target? Gut. 2020;69(5):841–851. http://dx.doi.org/10.1136/gutjnl-2019-318512
Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, et al. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol. 2020;5(5):426-428. https://doi.org/10.1016/S2468-1253(20)30076-5
Brenner EJ, Ungaro RC, Colombel JF, Kappelman MD. Surveillance Epidemiology of Coronavirus) Under Research Exclusion (SECURE-IBD) [acceso 15 de abril de 2020]. Database Public Data Update. Disponible en: https://www.covidibd.org
Fiorino G, Allocca M, Furfaro F, et al. Inflammatory bowel disease care in the COVID-19 pandemic era: the Humanitas, Milan experience. J Crohns Colitis. 2020. https://doi.org/10.1093/ecco-jcc/jjaa058
Rubin DT, Abreu MT, Rai V, Siegel CA; International Organization for the Study of Inflammatory Bowel Disease. Management of Patients with Crohn’s Disease and Ulcerative Colitis During the COVID-19 Pandemic: Results of an International Meeting. Gastroenterology. 2020; S0016-5085(20)30465-0. https://doi.org/10.1053/j.gastro.2020.04.002
World Health Organization [Internet]. Q&A on Coronaviruses [COVID-19]. [ acceso 15 de abril de 2020]. Disponible en: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
Danese S, Cecconi M, Spinelli A. Management of IBD during the COVID-19 outbreak: resetting clinical priorities. Nat Rev Gastroenterol Hepatol. 2020. https://doi.org/10.1038/s41575-020-0294-8
Shang L, Zhao J, Hu Y, Du R, Cao B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet. 2020; 395:683–4. https://doi,org/10.1016/S0140-6736(20)30361-5
Gu J, Han B, Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission [published online ahead of print, 2020 Mar 3]. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.02.054
Chen L, Lou J, Bai Y, Wang M. COVID-19 Disease with Positive Fecal and Negative Pharyngeal and Sputum Viral Tests [published online ahead of print, 2020 Mar 20]. Am J Gastroenterol. 2020. https://doi.org/10.14309/ajg.0000000000000610
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020. https://doi,org/10.1038/s41586-020-2196-x
Sultan S, Lim JK, Altayar O, Davitkov P, Feuerstein JD, Siddique SM, et al. AGA Institute Rapid Recommendations for Gastrointestinal Procedures During the COVID-19 Pandemic. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.03.072
Repici A, Maselli R, Colombo M, Spadaccini M, Anderloni A, Carrara S, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020. https://doi.org/10.1016/j.gie.2020.03.019
Sociedad Española de Endoscopia Digestiva (SEED). Recomendaciones de la SEED: Protección en Unidades de Endoscopia frente al COVID-19 [Internet] [acceso 15 de abril de 2020]. Disponible en: https://wseed.es/images/site/guia_clinica/2020/RecomendacionesSEED_ProteccionUnidadesEndoscopia_Coronavirus.pdf
Zhang Y, Zhang X, Liu L, Wang H, Zhao Q. Suggestions for infection prevention and control in digestive endoscopy during current 2019-nCoV pneumonia outbreak in Wuhan, Hubei province, China. Endoscopy. 2020;52(4):312–314. https://doi.org/10.1055/a-1128-4313
Otero W, Gómez M, Ángel LA, Ruiz O, Marulanda H, Riveros J, et al. Procedimientos endoscópicos y pandemia COVID-19 Consideraciones básicas. Rev Colomb Gastroenterol. 2020;35(1):65-75. https://doi.org/10.22516/25007440.526
Rubin DT, Feuerstein JD, Wang AY, Cohen RD. AGA Clinical Practice Update on Management of Inflammatory Bowel Disease During the COVID-19 Pandemic: Expert Commentary. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.04.012
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















