Differences in Gastroenterology Procedure Rates in Colombia According to Geographic Location and Health Insurance Regimen
DOI:
https://doi.org/10.22516/25007440.1407Keywords:
Diagnostic techniques and procedures, surgical procedures of the digestive system, gastroenterology, barriers to healthcare AccessAbstract
Introduction: Previous evidence suggests the existence of barriers that may result in differential access to healthcare in Colombia; however, the impact on diagnostic gastroenterology procedures has not been evaluated.
Objectives: To assess procedure rates (PR) in gastroenterology and describe differences according to geographic location, insurance regimen, age, and sex.
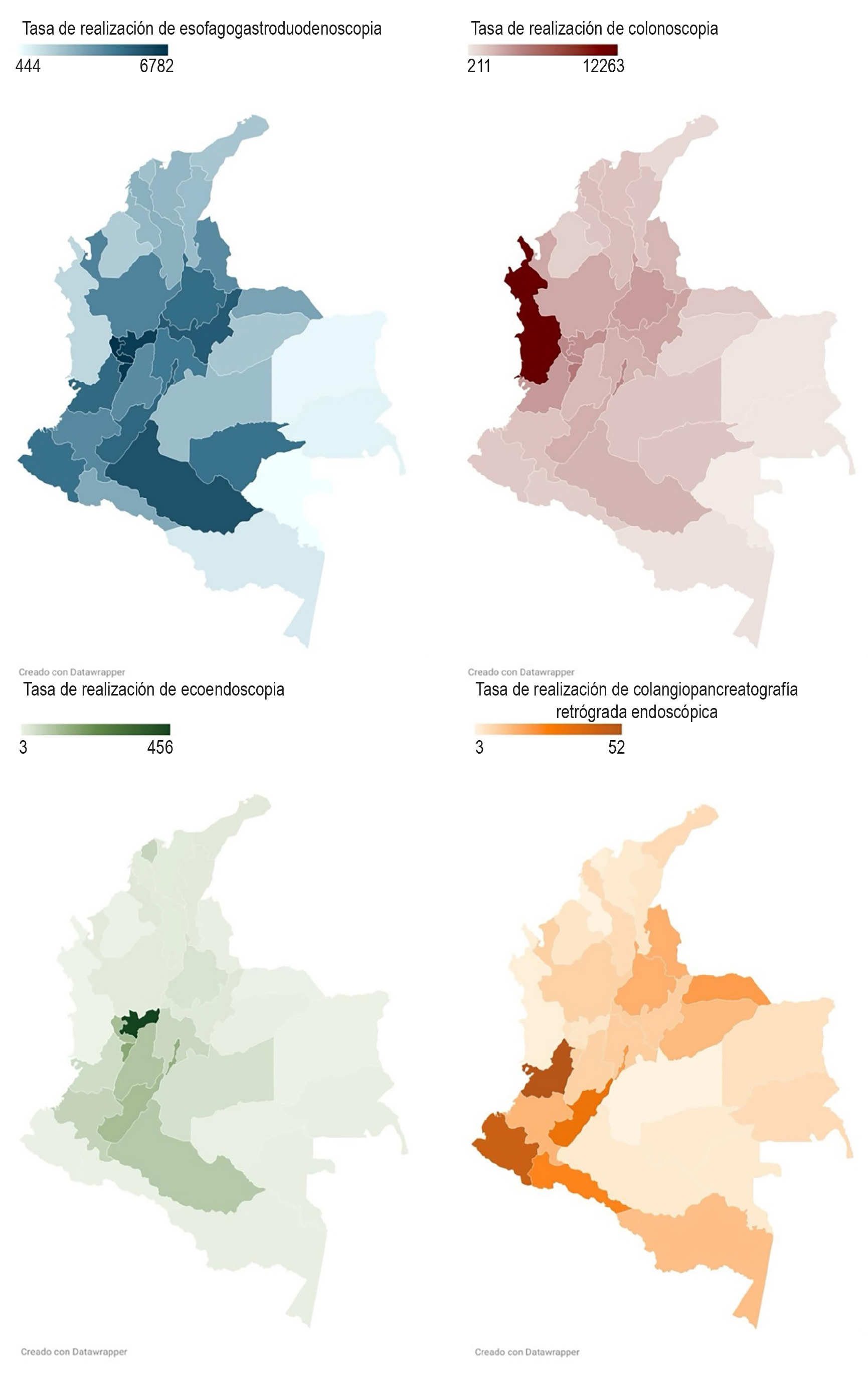
Methods: Secondary analysis of a population-based database containing data reported to the Integrated Social Protection Information System (SISPRO) in Colombia between 2017 and 2023. PRs were calculated for esophagogastroduodenoscopy (EGD), colonoscopy, endoscopic ultrasound (EUS), and endoscopic retrograde cholangiopancreatography (ERCP). Procedure rate ratios (PRRs) were computed according to geographic region, sex, and insurance regimen.
Results: National PRs ranged from 66 per 100,000 inhabitants for EUS to 4,144 per 100,000 for EGD, with significantly lower rates in the Caribbean coast, southern, and eastern regions of Colombia. PRs were higher in women (PRR EGD: 1.66; confidence interval [CI]: 1.65–1.66; p < 0.001; PRR ERCP: 1.52; CI: 1.45–1.59; p < 0.001) and lower in patients under the subsidized insurance regimen (PRR ERCP: 0.85; CI: 0.82–0.89; p < 0.0001; PRR EUS: 0.50; CI: 0.49–0.51; p < 0.0001). A progressive increase in procedure rates with age was observed.
Conclusions: Our findings indicate that procedure rates increase with age and are higher in women. Furthermore, patients residing in certain geographic areas of Colombia and those enrolled in the subsidized insurance regimen face barriers to accessing gastroenterology procedures. These results underscore the need to implement public health policies aimed at reducing these disparities.
Downloads
References
Bejarano M, Gallego CX, Gómez JR. Frecuencia de abdomen agudo quirúrgico en pacientes que consultan al servicio de urgencias. Rev Colomb Cir. 2011;26:33-41.
Páramo Hernández DB, Albis R, Galiano MT, Mendoza de Molano B, Rincón R, Pineda Ovalle LF, et al. Prevalencia de síntomas del reflujo gastroesofágico y factores asociados: una encuesta poblacional en las principales ciudades de Colombia. Rev. colomb. Gastroenterol. 2017;31(4):337-46. https://doi.org/10.22516/25007440.108
Pontet Y, Olano C. Prevalencia de síndrome de intestino irritable en América Latina. Rev Gastroenterol Perú. 2021;41(3):144-149. https://doi.org/10.47892/rgp.2021.413.1154
Sepúlveda Copete M, Maldonado Gutiérrez C, Bravo Ocaña JC, Satizabal N, Gempeler Rojas A, Castro Llanos AM, et al. Prevalencia de Helicobacter pylori en pacientes llevados a endoscopia de vías digestivas altas en un hospital de referencia en Cali, Colombia, en 2020. Rev Colomb Gastroenterol. 2022;37(4):355-61. https://doi.org/10.22516/25007440.868
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249. https://doi.org/10.3322/caac.21660
Vreeburg EM, Terwee CB, Snel P, Rauws EA, Bartelsman JF, Meulen JH, et al. Validation of the Rockall risk scoring system in upper gastrointestinal bleeding. Gut. 1999;44(3):331-5. https://doi.org/10.1136/gut.44.3.331
An Z, Braseth AL, Sahar N. Acute Cholangitis: Causes, Diagnosis, and Management. Gastroenterol Clin North Am. 2021;50(2):403-414. https://doi.org/10.1016/j.gtc.2021.02.005
Mora-Moreo L, Estrada-Orozco K, Espinosa O, Melgarejo LM. Characterization of the population affiliated to the subsidized health insurance scheme in Colombia: a systematic review and meta-analysis. Int J Equity Health. 2023;22(1):28. https://doi.org/10.1186/s12939-022-01818-x
Parra-Lara L, Falla-Martinez J, Bravo J, Bravo L, Zambrano A. Health disparities and gastric cancer survival in Cali, Colombia: a hospital-based study. Annals Of Oncology. 2019;30:iv94. https://doi.org/10.1093/annonc/mdz155.340
Hilarión-Gaitán L, Díaz-Jiménez D, Cotes-Cantillo K, Castañeda-Orjuela C. Desigualdades en salud según régimen de afiliación y eventos notificados al Sistema de Vigilancia (Sivigila) en Colombia, 2015. Biomédica. 2019;39(4):737-747. https://doi.org/10.7705/biomedica.4453
Ministerio de Salud y Protección Social. Contenido tabla de referencia CUPS [Internet]. SISPRO [consultado el 4 de febrero de de 2025]. Disponible en: https://web.sispro.gov.co/WebPublico/Consultas/ConsultarDetalleReferenciaBasica.aspx?Code=CUPS
Ministerio De Salud y Protección Social. Resolución número 2077 de 2021, por la cual se establece la Clasificación Única de Procedimientos en Salud – CUPS [Internet]. Ministerio De Salud y Protección Social; 2021 [consultado el 4 de febrero de de 2025]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-2077-de-2021.pdf
Ruhl CE, Everhart JE. Indications and outcomes of Gastrointestinal Endoscopy. En: Everhart JE (editor). The Burden of Digestive Diseases in the United States. Washington, DC: US Government Printing Office; 2008. p. 123-36.
García-Rodríguez A, Fernández-Esparrach G, Sendino O, Ginès A; en representación del Grupo de Ecoendoscopia de la SEED. State of endoscopic ultrasonography in Spain in 2017. Gastroenterol Hepatol. 2018;41(10):672-678. https://doi.org/10.1016/j.gastrohep.2018.06.009
Houghton N, Báscolo E, Jara L, Cuellar C, Coitiño A, Del Riego A, et al. Barreras de acceso a los servicios de salud para mujeres, niños y niñas en América Latina. Rev Panam Salud Publica. 2022;46:e94. https://doi.org/10.26633/RPSP.2022.94
Mayer EA, Naliboff B, Lee O, Munakata J, Chang L. Review article: gender-related differences in functional gastrointestinal disorders. Aliment Pharmacol Ther. 1999;13 Suppl 2:65-9. https://doi.org/10.1046/j.1365-2036.1999.00008.x
Zhu H, Ji K, Wu W, Zhao S, Zhou J, Zhang C, et al. Describing Treatment Patterns for Elderly Patients with Intrahepatic Cholangiocarcinoma and Predicting Prognosis by a Validated Model: A Population-Based Study. J Cancer. 2021;12(11):3114-3125. https://doi.org/10.7150/jca.53978
Rodríguez-González FJ, Naranjo-Rodríguez A, Mata-Tapia I, Chicano-Gallardo M, Puente-Gutiérrez JJ, López-Vallejos P, et al. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58(2):220-5. https://doi.org/10.1067/mge.2003.363
Gaitán JA, Martínez VM. Enfermedad litiásica biliar, experiencia en una clínica de cuarto nivel, 2005-2011. Rev Colomb Cir. 2014;29(3):188-96. https://doi.org/10.30944/20117582.397
Alvis-Zakzuk J, Marrugo-Arnedo C, Alvis-Zakzuk NJ, De la Rosa FG, Florez-Tanus Á, Moreno-Ruiz D, et al. Gasto de bolsillo y gasto catastrófico en salud en los hogares de Cartagena, Colombia. Rev Salud Pública. 2018;20(5):591-8. https://doi.org/10.15446/rsap.v20n5.61403
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















