Comparative Evaluation of the Glasgow-Blatchford, Pre-Endoscopic Rockall, and CANUKA Scores in Predicting Morbidity in Patients with Upper Gastrointestinal Bleeding
DOI:
https://doi.org/10.22516/25007440.1360Keywords:
Gastrointestinal hemorrhage, morbidity, comparativeAbstract
Introduction and Objective: Upper gastrointestinal bleeding (UGIB) is a common reason for presentation in emergency departments. Various scoring systems have been developed to determine the need for endoscopic intervention and to predict the risk of adverse outcomes. The aim of this study was to evaluate the Glasgow-Blatchford score (GBS), CANUKA score, and pre-endoscopic Rockall score as predictors of a composite morbidity outcome in patients with non-variceal UGIB.
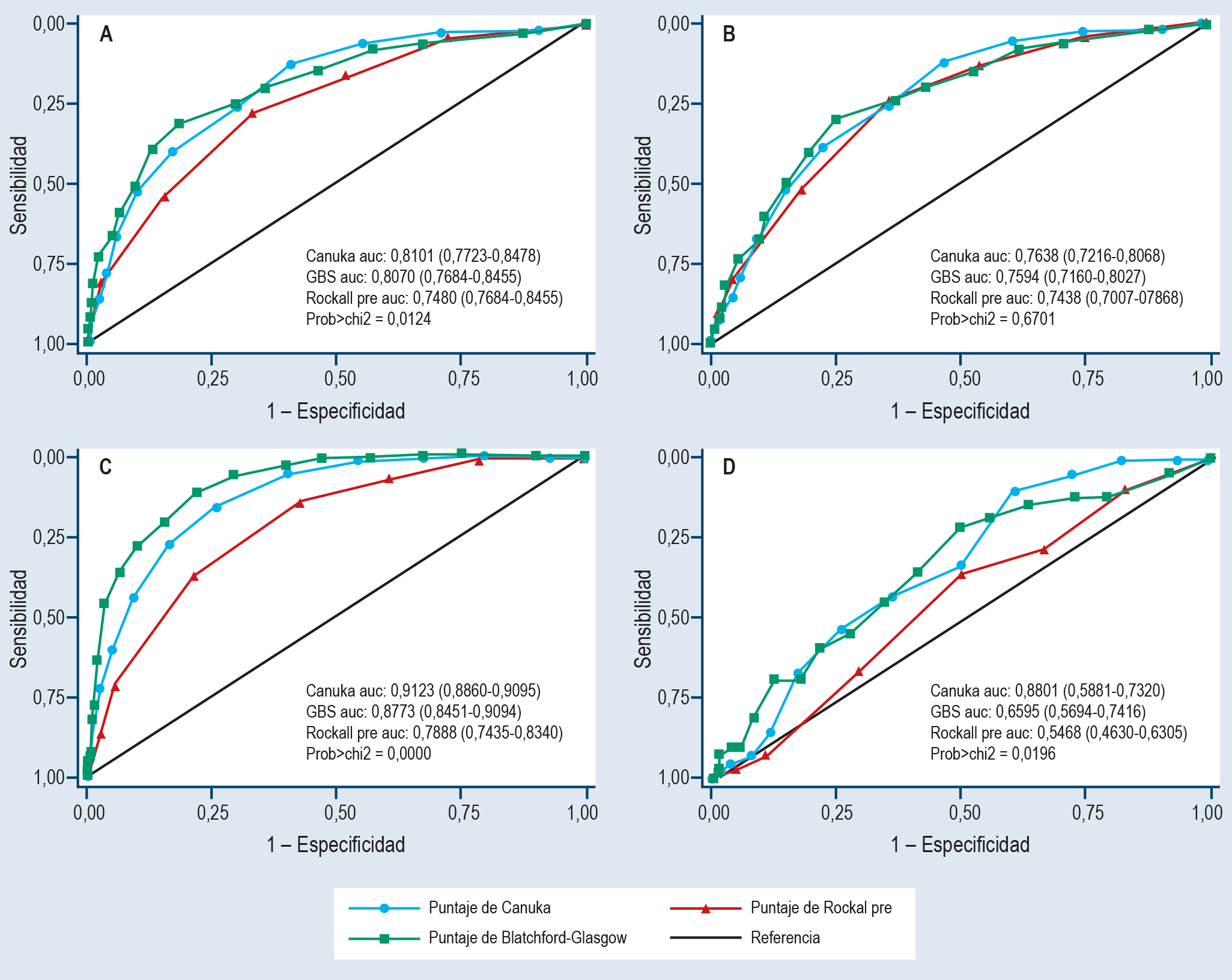
Materials and Methods: This retrospective study included patients with non-variceal UGIB and compared the discriminative ability of three scoring systems to predict a composite morbidity outcome, defined as a hospital stay exceeding 72 hours, intensive care unit (ICU) admission, need for endoscopic hemostatic therapy, blood product transfusion, embolization, repeat endoscopic intervention, or surgical management. Areas under the curve (AUC) were compared using DeLong’s method.
Results: A total of 496 patients were included (median age: 60 years; 62.3% male; 20.6% with cancer). The composite morbidity outcome occurred in 49.4% of patients, and 3.23% died. The CANUKA (AUC: 0.8101) and GBS (AUC: 0.8070) scores demonstrated superior discriminative ability (p = 0.0124). Individually, the GBS showed the best capacity to discriminate patients requiring ICU care (AUC: 0.8011; p = 0.0004) and blood product transfusion (AUC: 0.9123; p < 0.0001). Both CANUKA and GBS scores were superior in predicting the need for repeat endoscopic intervention, with AUROC values of 0.6601 and 0.6555, respectively.
Conclusion: These findings suggest that the CANUKA and GBS scores are superior predictors of morbidity and should be preferred when making decisions regarding early intervention and close monitoring.
Downloads
References
Oakland K. Changing epidemiology and etiology of upper and lower gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2019;42-43:101610. https://doi.org/10.1016/j.bpg.2019.04.003
Tielleman T, Bujanda D, Cryer B. Epidemiology and Risk Factors for Upper Gastrointestinal Bleeding. Gastrointest Endosc Clin N Am. 2015;25(3):415-28. https://doi.org/10.1016/j.giec.2015.02.010
Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. American Journal of Gastroenterology. 2021;116(5):899-917. https://doi.org/10.14309/ajg.0000000000001245
Gralnek IM, Stanley AJ, Morris AJ, Camus M, Lau J, Lanas A, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2021. Endoscopy. 2021;53(3):300-32. https://doi.org/10.1055/a-1369-5274
Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38(3):316-21. https://doi.org/10.1136/gut.38.3.316
Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper gastrointestinal haemorrhage. The Lancet. 2000;356(9238):1318-21. https://doi.org/10.1016/S0140-6736(00)02816-6
Oakland K, Kahan BC, Guizzetti L, Martel M, Bryant RV, Brahmania M, et al. Development, Validation, and Comparative Assessment of an International Scoring System to Determine Risk of Upper Gastrointestinal Bleeding. Clinical Gastroenterology and Hepatology. 2019;17(6):1121-1129.e2. https://doi.org/10.1016/j.cgh.2018.09.039
Bryant RV, Kuo P, Williamson K, Yam C, Schoeman MN, Holloway RH, et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc. 2013;78(4):576-83. https://doi.org/10.1016/j.gie.2013.05.003
Taha AS, McCloskey C, Craigen T, Angerson WJ. Antithrombotic drugs and non-variceal bleeding outcomes and risk scoring systems: comparison of Glasgow Blatchford, Rockall and Charlson scores. Frontline Gastroenterol. 2016;7(4):257-63. https://doi.org/10.1136/flgastro-2015-100671
Li Y, Lu Q, Song M, Wu K, Ou X. Comparisons of six endoscopy independent scoring systems for the prediction of clinical outcomes for elderly and younger patients with upper gastrointestinal bleeding. BMC Gastroenterol. el 2022;22(1):187. https://doi.org/10.1186/s12876-022-02266-1
Stata Corp. Stata 16 [Software]. Stata; 2019 [consultado el diciembre 30 del 2019]. Disponible en: https://www.stata.com/stata16/
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics. 1988;44(3):837. https://doi.org/10.2307/2531595
Stanley AJ, Laine L, Dalton HR, Ngu JH, Schultz M, Abazi R, et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: international multicentre prospective study. BMJ. 2017:356:i6432. https://doi.org/10.1136/bmj.i6432
Lincoln M, Keating N, O’Loughlin C, Tam A, O’Kane M, MacCarthy F, et al. Comparison of risk scoring systems for critical care patients with upper gastrointestinal bleeding: predicting mortality and length of stay. Anaesthesiol Intensive Ther. 2022;54(4):310-4. https://doi.org/10.5114/ait.2022.120741
Cassana A, Scialom S, Segura E, Chacaltana A. Estudio de validación diagnóstica de la escala de Glasgow-Blatchfordpara la predicción de mortalidad en pacientes con hemorragia digestiva alta en un hospital de Lima, Perú (junio 2012-diciembre 2013). Rev Esp Enferm Dig. 2015;107(8):476-82. https://doi.org/10.17235/reed.2015.3745/2015
Aktas G, Ustaoglu M, Bakir T, Aslan R, Goren F, Bektas A. Analysis of the patients with nonvariceal upper gastrointestinal bleeding and comparison of Rockall and Glasgow-Blatchford scores. Indian Journal of Gastroenterology. 2022;41(6):576–82. https://doi.org/10.1007/s12664-022-01290-z
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















