Prevalence of Achalasia in Colombia: Data from the Official Records of the Ministry of Health, 2017–2024
DOI:
https://doi.org/10.22516/25007440.1349Keywords:
Esophageal achalasia, epidemiology, prevalence, ColombiaAbstract
Introduction: The global prevalence of achalasia is low, estimated at between 7 and 32 cases per 100,000 inhabitants. Colombia is an endemic country for Chagas disease, and variants of the human leukocyte antigen DQ (HLA-DQ) have also been identified in the population. These factors may influence the disease’s prevalence compared to global figures.
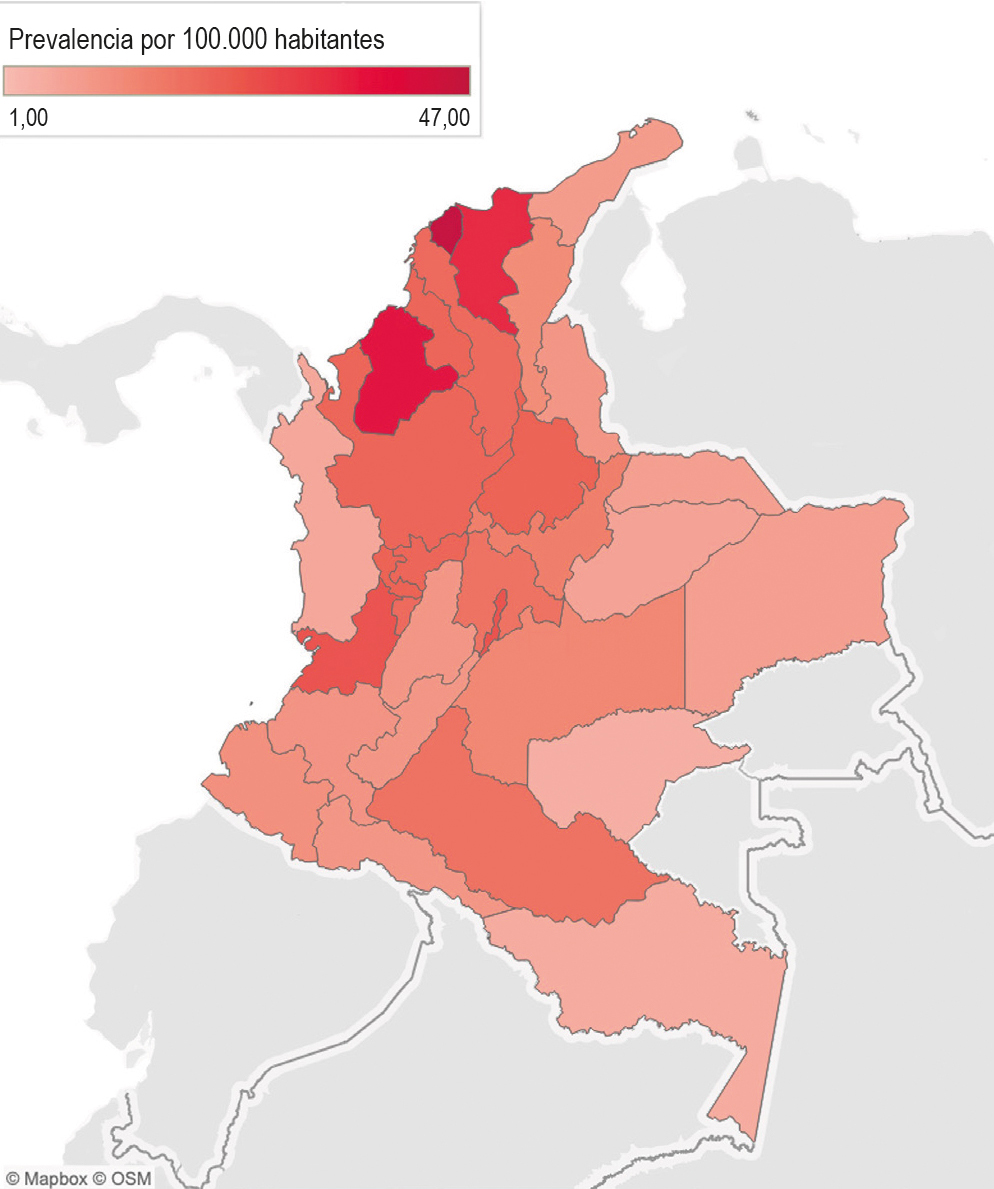
Methods: This was a descriptive, cross-sectional study based on information from the database of Integrated Information System for Social Protection of Colombia (SISPRO). Prevalence was estimated based on healthcare encounters coded with ICD-10 diagnosis K22.0, corresponding to “achalasia of the cardia,” during the period from 2017 to 2024. The analysis was stratified by department, sex, and age group.
Results: A total of 9,621 cases of achalasia were recorded nationwide, with a prevalence of 21.8 cases per 100,000 inhabitants. Females accounted for 59.4% of the cases (95% CI: 58.4%–60.4%). The departments with the highest prevalence were Atlántico, Córdoba, Magdalena, and Bogotá, with 47, 39, 35, and 26 cases per 100,000 inhabitants, respectively. A progressively higher prevalence was observed with increasing age.
Conclusions: The estimated prevalence of the disease in Colombia aligns with global reports. Further studies are needed to confirm geographic differences in prevalence and their possible underlying causes. These findings are useful for prioritizing resources and improving strategies for the detection and treatment of achalasia in Colombia.
Downloads
References
Savarino EBS, Roman S, Sifrim D, Tack J, Thompson SK, Gyawali CP. Achalasia. Nat Rev Dis Primers. 2022;8(1):28. https://doi.org/10.1038/s41572-022-00356-8
Wu XY, Liu ZQ, Wang Y, Chen WF, Gao PT, Li QL, et al. The etiology of achalasia: An immune-dominant disease. J Dig Dis. 2021;22(3):126-135. https://doi.org/10.1111/1751-2980.12973
Li MY, Wang QH, Chen RP, Su XF, Wang DY. Pathogenesis, clinical manifestations, diagnosis, and treatment progress of achalasia of cardia. World J Clin Cases. 2023;11(8):1741-1752. https://doi.org/10.12998/wjcc.v11.i8.1741
Pandolfino JE, Gawron AJ. Achalasia: A systematic review. JAMA. 2015;313(18):1841. https://doi.org/10.1001/jama.2015.2996
Costigan DJ, Clouse RE. Achalasia-like esophagus from amyloidosis: Successful treatment with pneumatic bag dilatation. Dig Dis Sci. 1983;28(8):763-5. https://doi.org/10.1007/BF01312569
Foster PN, Stewart M, Lowe JS, Atkinson M. Achalasia like disorder of the oesophagus in von Recklinghausen’s neurofibromatosis. Gut. 1987;28(11):1522-6. https://doi.org/10.1136/gut.28.11.1522
Roberts DH, Gilmore IT. Achalasia in Anderson-fabry’s disease. J R Soc Med. 1984;77(5):430-1. https://doi.org/10.1177/014107688407700520
Miller HJ, Neupane R, Fayezizadeh M, Majumder A, Marks JM. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc. 2017;31(4):1636-42. https://doi.org/10.1007/s00464-016-5151-z
Lee K, Hong SP, Yoo IK, Yeniova AÖ, Hahn JW, Kim MS, et al. Global trends in incidence and prevalence of achalasia, 1925-2021: A systematic review and meta‐analysis. United European Gastroenterol J. 2024;12(4):504-15. https://doi.org/10.1002/ueg2.12555
Rosselli D, Pantoja-Ruiz C. SISPRO: The administrative database of the Colombian healthcare system. Acta Neurol Colomb. 2022;38(4):187-190. https://doi.org/10.22379/24224022426
Fernández-Ávila DG, Rincón-Riaño DN, Bernal-Macías S, Gutiérrez-Dávila JM, Rosselli D. Prevalence of rheumatoid arthritis in Colombia based on information from the Ministry of Health registry. Rev Colomb Reumatol. 2019;26(2):83-87. https://doi.org/10.1016/j.rcreue.2019.01.009
Otálora Esteban JF, Hernández Meza JS, Rosselli Cock DA. Epidemiología de la colecistitis aguda en Colombia: un análisis de los registros oficiales del Ministerio de Salud. Rev Colomb Gastroenterol. 2024;39(3):267-72. https://doi.org/10.22516/25007440.1166
Departamento Nacional del Planeación. Aseguramiento de Población [Internet]. Departamento Nacional del Planeación; 2024 [consultado el 19 de enero de 2025]. Disponible en: https://www.dnp.gov.co/LaEntidad_/subdireccion-general-prospectiva-desarrollo-nacional/direccion-desarrollo-social/Paginas/aseguramiento-de-poblacion.aspx#:~:text=Los%20esfuerzos%20mencionados%20han%20incidido,99%2C12%25%20en%202022
Departamento Administrativo Nacional de Estadística. Censo nacional de población y vivienda 2018 [Internet]. DANE; 2022 [consultado el 19 de enero de 2025]. Disponible en: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/censo-nacional-de-poblacion-y-vivenda-2018
Tableau. Business Intelligence and Analytics Software [Internet]. Tableau [consultado el 19 de enero de 2025]. Disponible en: https://www.tableau.com/
Sato H, Yokomichi H, Takahashi K, Tominaga K, Mizusawa T, Kimura N, et al. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol. 2019:54;621-7. https://doi.org/10.1007/s00535-018-01544-8
Van Hoeij FB, Ponds FA, Smout AJ, Bredenoord AJ. Incidence and costs of achalasia in The Netherlands. Neurogastroenterol Motil. 2018;30(2):10.1111/nmo.13195. https://doi.org/10.1111/nmo.13195
Samo S, Carlson DA, Gregory DL, Gawel SH, Pandolfino JE, Kahrilas PJ. Incidence and Prevalence of Achalasia in Central Chicago, 2004-2014, Since the Widespread Use of High-Resolution Manometry. Clin Gastroenterol Hepatol. 2017;15(3):366-373. https://doi.org/10.1016/j.cgh.2016.08.030
Guarnizo-Herreño CC, Agudelo C. Equidad de género en el acceso a los servicios de salud en Colombia. Rev Salud Publica. 2008;10(Supl 1):44-57. https://doi.org/10.1590/S0124-00642008000600005
Samo S, Carlson DA, Gregory DL, Gawel SH, Pandolfino JE, Kahrilas PJ. Incidence and prevalence of achalasia in central Chicago, 2004-2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol. 2017;15(3):366-73. https://doi.org/10.1016/j.cgh.2016.08.030
Instituto Nacional de Salud. Enfermedad de Chagas, Colombia 2023 [Internet]. Bogotá: Boletín Epidemiológico Semanal - Instituto Nacional de Salud; 2024 [consultado el 15 de diciembre de 2024]. Disponible en: https://www.ins.gov.co/buscador-eventos/BoletinEpidemiologico/2024_Bolet%C3%ADn_epidemiologico_semana_14.pdf https://doi.org/10.33610/23576189.2024.14
Instituto Nacional de Salud. Cáncer en menores de 18 años. Comportamiento epidemiológico, Colombia, 2023 [Internet]. Bogotá: Boletín Epidemiológico Semanal - Instituto Nacional de Salud; 2024 [consultado el 15 de diciembre de 2024]. Disponible en: https://www.ins.gov.co/buscador-eventos/BoletinEpidemiologico/2024_Boletin_epidemiologico_semana_34.pdf https://doi.org/10.33610/23576189.2024.06
Panesso-Gómez S, Pavia P, Rodríguez-Mantilla IE, Lasso P, Orozco LA, Cuellar A, et al. Trypanosoma cruzi Detection in Colombian Patients with a Diagnosis of Esophageal Achalasia. Am J Trop Med Hyg. 2018;98(3):717-723. https://doi.org/10.4269/ajtmh.17-0417
Latiano A, De Giorgio R, Volta U, Palmieri O, Zagaria C, Stanghellini V, et al. HLA and enteric antineuronal antibodies in patients with achalasia. Neurogastroenterol Motil. 2006;18(7):520-5. https://doi.org/10.1111/j.1365-2982.2006.00772.x
Ruiz de León A, Mendoza J, Sevilla-Mantilla C, Fernández AM, Pérez-de-la-Serna J, Gónzalez VA, et al. Myenteric antiplexus antibodies and class II HLA in achalasia. Dig Dis Sci. 2002;47(1):15-9. https://doi.org/10.1023/A:1013242831900
Furuzawa-Carballeda J, Zuñiga J, Hernández-Zaragoza DI, Barquera R, Marques-García E, Jiménez-Alvarez L, et al. An original Eurasian haplotype, HLA-DRB1*14:54-DQB1*05:03, influences the susceptibility to idiopathic achalasia. PLoS One. 2018;13(8):e0201676. https://doi.org/10.1371/journal.pone.0201676
Hernández-Mejía DG, Páez-Gutiérrez IA, Dorsant Ardón V, Camacho Ramírez N, Mosquera M, Cendales PA, et al. Distributions of the HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1 alleles and haplotype frequencies of 1763 stem cell donors in the Colombian Bone Marrow Registry typed by next-generation sequencing. Front Immunol. 2023;13:1057657. https://doi.org/10.3389/fimmu.2022.1057657
Arrué-Hernández KA, Soto-Cáceres VA, Fernández-Mogollón JL. Características del registro y codificación diagnóstica de los pacientes hospitalizados en un hospital del seguro social de Chiclayo. Rev Cuerpo Med HNAAA. 2019;12(1):13-8.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















