Mortality and Futility in Patients Undergoing Gastrostomy Between 2020 and 2023
DOI:
https://doi.org/10.22516/25007440.1295Keywords:
Gastrostomy, treatment futility, SARS-CoV-2, mortality, bioethicsAbstract
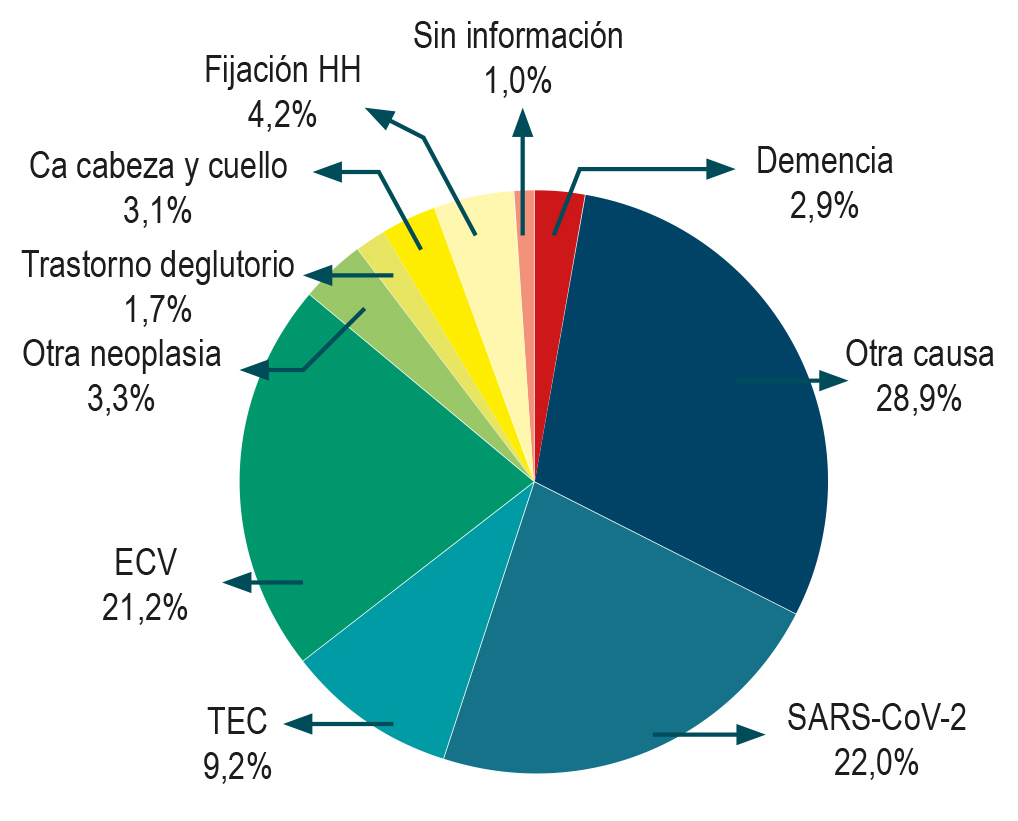
Gastrostomy is a common procedure in hospitals and clinics, typically associated with a low complication rate, and is performed in patients requiring long-term artificial feeding. In daily clinical practice, uncertainty often arises regarding the potential futility of some of these procedures, particularly given the poor vital and functional prognosis of many patients who require them. This study collected data on patients who underwent gastrostomy between 2020 and 2023 at a tertiary care institution, aiming to quantify in-hospital mortality and determine the proportion of procedures deemed futile. Futility in this context was defined as the performance of gastrostomy in patients with advanced dementia, a persistent vegetative state, or death within the first week following the procedure. Overall, in-hospital mortality was found to be 13.1%, and 10.4% of gastrostomies were considered futile. Additionally, higher rates of procedure-related complications and in-hospital deaths were observed during the COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A downward trend in futile procedures was noted following the implementation of an institutional protocol on the subject during the study period.
Downloads
References
Tae CH, Lee JY, Joo MK, Park CH, Gong EJ, Shin CM, et al. Clinical practice guidelines for percutaneous endoscopic gastrostomy. Clin Endosc. 2023;56(4):391-408. https://doi.org/10.5946/ce.2023.062
Dietrich CG, Schoppmeyer K. Percutaneous endoscopic gastrostomy - Too often? Too late? Who are the right patients for gastrostomy? World J Gastroenterol. 2020;26(20):2464-71. https://doi.org/10.3748/wjg.v26.i20.2464
Hoyos JB. La futilidad como criterio médico, la prudencia como valor para mediar en la justicia de la atención de pacientes al final de la vida. Meridiano. 2022;1(2):2-12. https://doi.org/10.26852/28059107.625
Congreso de Colombia. Ley 23 de 1981, por la cual se dictan normas en materia de ética médica [Internet]. Congreso de Colombia; 1981 [consultado el 10 de diciembre de 2024]. Disponible en: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=68760
Knight Alzheimer Disease Research Center. CDR® Dementia Staging Instrument [Internet]. WashU Medicine Department of Neurology [citado 10 de diciembre de 2024]. Disponible en: https://knightadrc.wustl.edu/professionals-clinicians/cdr-dementia-staging-instrument/
Lima DL, Miranda LEC, Lima RNCL, Romero-Velez G, Chin R, Shadduck PP, et al. Factors Associated with Mortality after Percutaneous Endoscopic Gastrostomy. JSLS. 2023;27(2):e2023.00005. https://doi.org/10.4293/JSLS.2023.00005
Pih GY, Na HK, Ahn JY, Jung KW, Kim DH, Lee JH, et al. Risk factors for complications and mortality of percutaneous endoscopic gastrostomy insertion. BMC Gastroenterol. 2018;18(1):101. https://doi.org/10.1186/s12876-018-0825-8
Sako A, Yasunaga H, Horiguchi H, Fushimi K, Yanai H, Uemura N. Prevalence and in-hospital mortality of gastrostomy and jejunostomy in Japan: a retrospective study with a national administrative database. Gastrointest Endosc. 2014;80(1):88-96. https://doi.org/10.1016/j.gie.2013.12.006
Stenberg K, Eriksson A, Odensten C, Darehed D. Mortality and complications after percutaneous endoscopic gastrostomy: a retrospective multicentre study. BMC Gastroenterol. 2022;22(1):361. https://doi.org/10.1186/s12876-022-02429-0
Stein DJ, Moore MB, Hoffman G, Feuerstein JD. Improving All-Cause Inpatient Mortality After Percutaneous Endoscopic Gastrostomy. Dig Dis Sci. 2021;66(5):1593-9. https://doi.org/10.1007/s10620-020-06396-y
Atencio DP, Blanco Pérez ÁG, Otero Regino W. Gastrostomía endoscópica percutánea en ancianos: indicaciones, seguridad y desenlaces. Rev Col Gastroenterol. 2015;30(1):3-10.
Culliane M, Gray AJG, Hargraves CMK, Lucas S, Schubert M, Sherry KM, et al. Scoping our Practice: The 2004 report of the national confidential enquiry into patient outcome and death [Internet]. Bristol, Inglaterra: NCEPOD; 2004 [consultado el 10 de diciembre de 2024]. Disponible en: https://www.ncepod.org.uk/2004report/Full_Report_2004.pdf
Kruse A, Misiewicz JJ, Rokkas T, Hammer H, Niv Y, Allison M, et al. Recommendations of the ESGE workshop on the Ethics of Percutaneous Endoscopic Gastrostomy (PEG) Placement for Nutritional Support. First European Symposium on Ethics in Gastroenterology and Digestive Endoscopy, Kos, Greece, June 2003. Endoscopy. 2003;35(9):778-80. https://doi.org/10.1055/s-2003-41589
Almonacid LT, Gómez M, Franco DMC, Rueda FEG, Quintero SR. Futilidad en cirugía: el caso de la gastrostomía. Rev Colomb Cir. 2020;35(3):429-35. https://doi.org/10.30944/20117582.728
Khaiser A, Baig M, Forcione D, Bechtold M, Puli SR. Efficacy and Safety of Peroral Endoscopic Myotomy (POEM) in Achalasia: An Updated Meta-analysis. Middle East J Dig Dis. 2023;15(4):235-41. https://doi.org/10.34172/mejdd.2023.352
Taxonera C, Olivares D, Alba C. Real-World Effectiveness and Safety of Tofacitinib in Patients With Ulcerative Colitis: Systematic Review With Meta-Analysis. Inflamm Bowel Dis. 2022;28(1):32-40. https://doi.org/10.1093/ibd/izab011
Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, et al. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology. 2016;150(5):1113-1124.e5. https://doi.org/10.1053/j.gastro.2016.01.028
Ardila-Suárez O. Aspectos éticos y médico legales relacionados con la realización de gastrostomía en adultos. Universidad CES; 2024 [consultado el 10 de diciembre de 2024]. Disponible en: https://repository.ces.edu.co/handle/10946/8644
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















