Incidence and Survival of Digestive Tract Cancer Detected by Endoscopy with Histological Confirmation in a High-Risk Region of Colombia
DOI:
https://doi.org/10.22516/25007440.1292Keywords:
Endoscopy, Cytopathology, Signs and Symptoms, Gastrointestinal neoplasms, survival analysisAbstract
Introduction: Cancers of the digestive tract are among the leading causes of mortality from non-communicable chronic diseases, both in Colombia and worldwide. These malignancies are often asymptomatic in their early stages, which significantly impacts survival rates and poses a major public health challenge. This study aimed to analyze survival rates following histopathological confirmation of digestive tract neoplasms detected through endoscopy at a regional referral center.
Methods: A retrospective cross-sectional study was conducted, reviewing biopsy results from endoscopies and colonoscopies performed between 2018 and 2020. Sociodemographic variables were analyzed, and survival rates were assessed using the Kaplan-Meier method and the Log-Rank test.
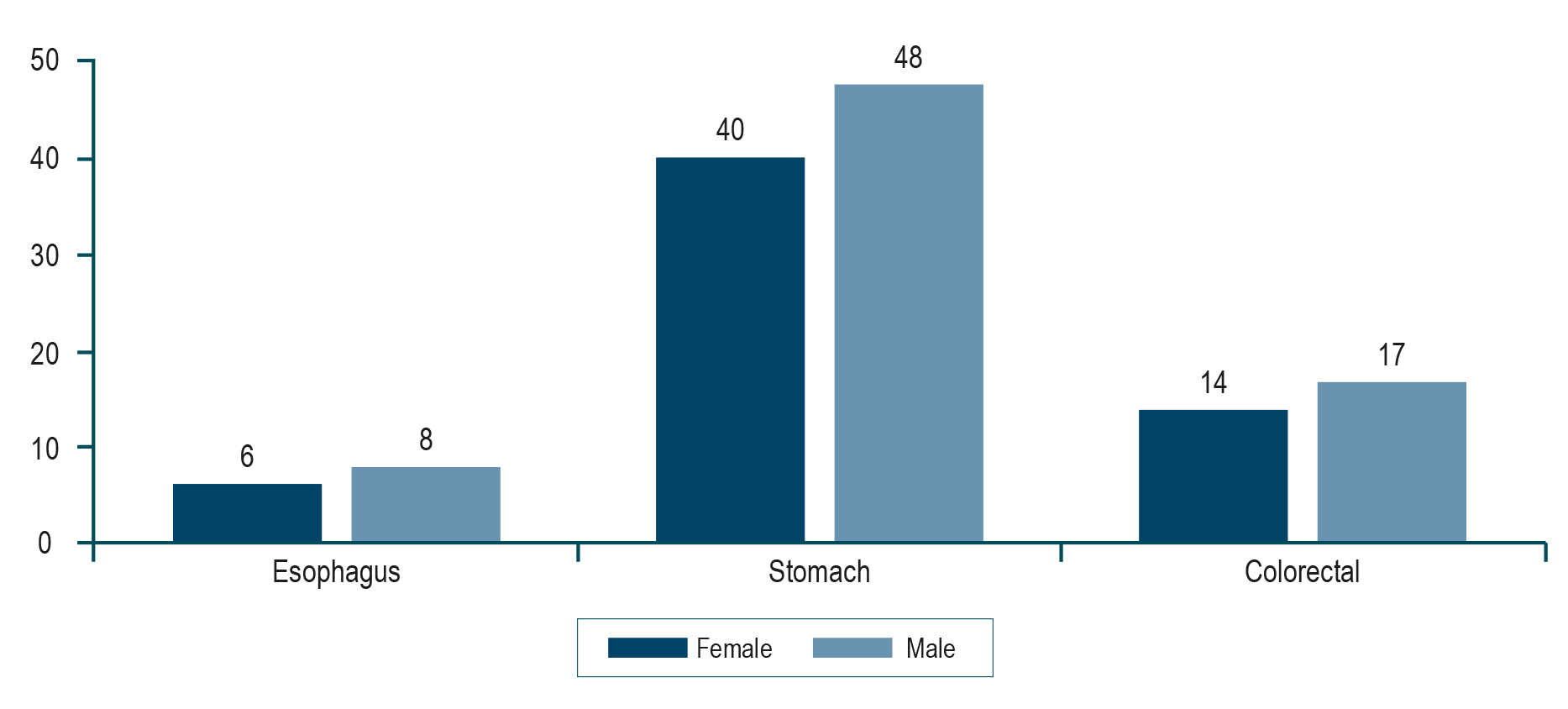
Results: A total of 133 cases of gastrointestinal neoplasms were identified: 66.1% in the stomach (n = 88), 23.3% in the colon (n = 31), and 10.6% in the esophagus (n = 14). The median age was 66.7 years (interquartile range [IQR]: 59–79), with a predominance of male patients. Follow-up data showed a median survival of five months from diagnosis to death, with a maximum survival of 2.3 years.
Conclusion: The majority of patients diagnosed with digestive tract cancer at the regional referral center were male and presented with advanced-stage disease, as reflected in the short survival times observed.
Downloads
References
Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, et al. Colombia cancer statistics for the year 2020: An overview. Int J Cancer. 2021;149(4):778-89. https://doi.org/10.1002/ijc.33588
Cancer (IARC). Global Cancer Observatory [Internet]. gco.iarc.fr. Disponible en: https://gco.iarc.who.int/
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12-49. https://doi.org/10.3322/caac.21820
Bravo LE, García LS, Collazos P, Carrascal E, Ramírez O, Collazos T, et al. Reliable information for cancer control in Cali, Colombia. Colomb Med. 2018;49(1):23-34. https://doi.org/10.25100/cm.v49i1.3689
Departamento Administrativo Nacional de Estadística. Defunciones no fetales 2023 [Internet]. [consultado el 21 de septiembre de 2024]. Disponible en: https://www.dane.gov.co/index.php/estadisticas-por-tema/salud/nacimientos-y-defunciones/defunciones-no-fetales/defunciones-no-fetales-2023
Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381(9864):400-12. https://doi.org/10.1016/S0140-6736(12)60643-6
De Vos-Geelen J, Geurts SME, Valkenburg-Van Iersel LBJ, De Jong EJM, Tjan-Heijnen VCG, Van Putten M, et al. Trends in treatment and overall survival among patients with proximal esophageal cancer. World J Gastroenterol. 2019;25(47):6835-46. https://doi.org/10.3748/wjg.v25.i47.6835
Hernández G. Epidemiología del cáncer en Colombia: una transicion que debemos conocer. Inst Nac Cancerol. 2021;43(1):64-73. https://doi.org/10.56050/01205498.1586
Correa P. Gastric cancer: overview. Gastroenterol Clin North Am. 2013;42(2):211-7. https://doi.org/10.1016/j.gtc.2013.01.002
Arias-Sosa LA, Cuspoca-Orduz AF, Siabato-Barrios JA, Eslava-Roa JS. Incidencia y mortalidad del cáncer gástrico en el departamento de Boyacá-Colombia. Acta Gastroenterol Latinoam. 2018;48(3):181-9.
Torres J, Correa P, Ferreccio C, Hernandez-Suarez G, Herrero R, Cavazza-Porro M, et al. Gastric cancer incidence and mortality is associated with altitude in the mountainous regions of Pacific Latin America. Cancer Causes Control. 2013;24(2):249-56. https://doi.org/10.1007/s10552-012-0114-8
Bravo LE, Collazos T, Collazos P, García LS, Correa P. Trends of cancer incidence and mortality in Cali, Colombia. 50 years experience. Colomb Med. 2012;43(4):246-55. https://doi.org/10.25100/cm.v43i4.1266
Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010-21. https://doi.org/10.1007/s12328-020-01237-x
Murphy N, Campbell PT, Gunter MJ. Unraveling the etiology of early-onset colorectal cancer. J Natl Cancer Inst. 2021;113(5):505-6. https://doi.org/10.1093/jnci/djaa165
Choi Y, Kim N, Yun CY, Choi YJ, Yoon H, Shin CM, et al. Effect of Helicobacter pylori eradication after subtotal gastrectomy on the survival rate of patients with gastric cancer: follow-up for up to 15 years. Gastric Cancer. 2020;23(6):1051-63. https://doi.org/10.1007/s10120-020-01076-2
Albero L, Arango A, Ríos AG, Elías C, Turriago P. Mortalidad por cánceres del aparato digestivo en Colombia entre 1980 y 1998. Análisis de tendencias y comparación reginal. Rev Fac Med. 2004;52(1):19-37.
Departamento Administrativo Nacional de Estadística. Encuesta Nacional de Consumo de Sustantcias Psicoativas (ENCSPA) 2019 [Internet]. [consultado el 22 de agosto de 2024]. Disponible en: https://www.dane.gov.co/files/investigaciones/boletines/ech/ech/CP_empleo_ago_22.pdf
IBM corp. IBM SPSS Statistics for Windows. IBM Corp., Armonk, NY, EE. UU.; 2017.
Sanz Anquela JM, Ruiz Liso JM, Rodríguez Manzanilla L, Alfaro Torres J, Almajano Martínez C, Cuervas-Mons Finat M, et al. Importancia de la clasificación de Laurén del cáncer gástrico. Revisión de una serie de 295 casos. Patología. 1989;22:156-161.
Lauren P. the Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. an Attempt At a Histo-Clinical Classification. Acta Pathol Microbiol Scand. 1965;64:31-49. https://doi.org/10.1111/apm.1965.64.1.31
Ministerio de Salud y Protección Social. Resolución 8430 de 1993, por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud [Internet]; [consultado el septiembre 15 de 2023]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.PDF
Bosman F, Carneiro F, Hruban R, Theise N. Who classification of tumours of the digestive system. 4.a edición. World Health Organization; 2010.
Bohorquez M, Sahasrabudhe R, Criollo A, Sanabria-Salas MC, Vélez A, Castro JM, et al. Clinical manifestations of colorectal cancer patients from a large multicenter study in Colombia. Medicine (Baltimore). 2016;95(40):e4883. https://doi.org/10.1097/MD.0000000000004883
Barrero DC, Cortés E, Rodríquez C, Didí-Cruz M. Características epidemiológicas y clínicas del cáncer colorrectal en pacientes de la ciudad de Ibagué durante el período 2000-2006. Rev Colomb Gastroenterol. 2008;23(4):315-26.
Ferreira EJ, Meléndez HJ. Características clínicas, demográficas e histopatológicas de los pacientes con cáncer colorrectal del Hospital Universitario de Santander. Rev Colomb Cirugía. 2012;27(3):213-20.
Campo-Sánchez SM, Camargo-Trillos J, Calle-Ramírez JA, Gómez-Wolff LR, Sánchez-Patiño LA, García-García HI. Colorectal cancer survival at an oncologic center in Colombia. A historic cohort study. Rev Gastroenterol México (Engl Ed). 2019;84(2):174-84. https://doi.org/10.1016/j.rgmx.2018.04.002
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-64. https://doi.org/10.3322/caac.21601
Global Cancer Observatory. Estimated number of deaths in 2020, worldwide, males, all ages [Internet]; [consultado el 16 de mayo de 2021]. Disponible en: https://gco.iarc.fr/
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-86. https://doi.org/10.1002/ijc.29210
Triana JJ, Aristizábal-Mayor JD, Plata MC, Medina M, Baquero L, Gil-Tamayo S, et al. Disease Burden of Gastric Cancer in Disability-Adjusted Life Years in Colombia. Rev Colomb Gastroenterol. 2017;32(4):326-31. https://doi.org/10.22516/25007440.175
Pardo C, De Vries E, Buitrago L, Gamboa Ó. Atlas de mortalidad por cáncer en Colombia [Internet]. Colombia: Instituto Nacional de Cancerología, Instituto Geográfico Agustín Codazzi; 2017 [consultado el 30 de julio de 2024]. Disponible en: https://www.ins.gov.co/TyS/programas-de-calidad/Documentos%20Programa%20EEDDCARIO/ATLAS_de_Mortalidad_por_cancer_en_Colombia.pdf
Vries E De, Uribe C, Pardo C, Lemmens V, Poel E Van De, Forman D, et al. Gastric cancer survival and affiliation to health insurance in a middle-income setting. Cancer Epidemiol. 2015;39(1):91-6. https://doi.org/10.1016/j.canep.2014.10.012
E.S.E. Hospital Universitario San Rafael de Tunja. Informe caracterización de grupos de valor y grupos de interés 2021 [Internet]. Tunja, Colombia: Hospital San Rafael de Tunja; 2022 [consultado el 20 de marzo de 2024]. Disponible en: https://www.hospitalsanrafaeltunja.gov.co/contenido.php?id=316&seccion=transparencia-y-acceso-a-la-informacion-publica&slug=informe-de-caracterizacion
Portillo Miño JD, Araujo Prado LM, Melo Yepes JM, Carlosama Rosero YH. Características sociodemográficas e histopatológicas en pacientes con cáncer gástrico en una población con alto riesgo en Colombia. Rev Colomb Gastroenterol. 2021;36(1):18-23. https://doi.org/10.22516/25007440.544
Jazieh AR, Akbulut H, Curigliano G, Rogado A, Alsharm AA, Razis ED, et al. Impact of the COVID-19 Pandemic on Cancer Care: A Global Collaborative Study. JCO Glob Oncol. 2020;(6):1428-38. https://doi.org/10.1200/GO.20.00351
Pamplona J, Solano R, Ramírez M, Durandez R, Mohamed F, Pardo L, et al. High prevalence of SARS-CoV-2 infection in patients scheduled for digestive endoscopy after the peak of the first wave of the pandemic. Gastroenterol Hepatol. 2021;44(9):614-619. https://doi.org/10.1016/j.gastrohep.2021.03.001.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















