Esophageal Leukoplakia and Its Clinical Significance: Does It Imply Risk?
DOI:
https://doi.org/10.22516/25007440.1279Keywords:
Leukoplakia, esophagus, esophageal diseases, epidermolytic hyperkeratosis, endoscopy, squamous cell carcinomaAbstract
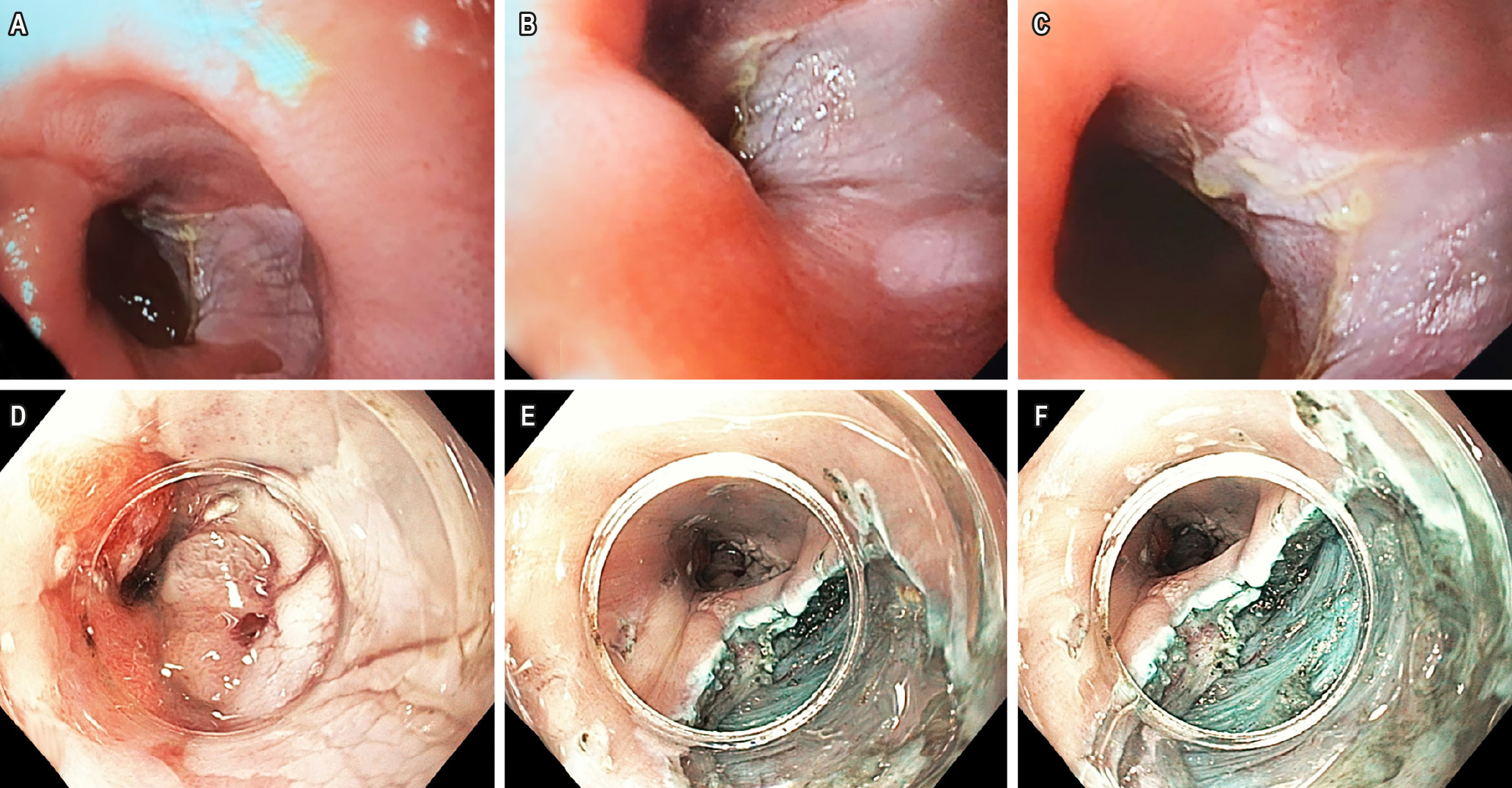
Esophageal leukoplakia is an extremely rare condition. It typically occurs in patients who smoke, frequently consume alcohol, or have chronic mucosal irritation from gastroesophageal reflux. Endoscopically, well-circumscribed whitish plaques are commonly observed in the middle or distal third of the esophagus. These lesions can be easily mistaken for glycogenic acanthosis, esophageal papilloma, eosinophilic esophagitis, or Candida esophagitis. Timely recognition and management are essential, as esophageal leukoplakia is considered a precursor to squamous cell carcinoma.
Downloads
References
Mello FW, Miguel AFP, Dutra KL, Porporatti AL, Warnakulasuriya S, Guerra ENS, et al. Prevalence of oral potentially malignant disorders: A systematic review and meta-analysis. J Oral Pathol Med. 2018;47(7):633-640. https://doi.org/10.1111/jop.12726
Park GB, Kim GH. Whitish plaques (leukoplakia) in the esophagus. Gastrointest Endosc. 2021;94(6):1144-1145. https://doi.org/10.1016/j.gie.2021.08.005
Singhi AD, Arnold CA, Crowder CD, Lam-Himlin DM, Voltaggio L, Montgomery EA. Esophageal leukoplakia or epidermoid metaplasia: A clinicopathological study of 18 patients. Mod Pathol 2014;27(1):38-43. https://doi.org/10.1038/modpathol.2013.100
Ashraf MF, Richter S, Arker SH, Parsa N. A Rare Case of Esophageal Leukoplakia: A Potential Precursor to Esophageal Malignancy. Cureus. 2021;13(8):e17205. https://doi.org/10.7759/cureus.17205
Johncilla ME, Srivastava A. Esophagitis unrelated to reflux disease: current status and emerging diagnostic challenges. Virchows Arch. 2018;472(1):29-41. https://doi.org/10.1007/s00428-017-2238-4
Kamboj AK, Gibbens YY, Hagen CE, Wang KK, Iyer PG, Katzka DA. Esophageal Epidermoid Metaplasia: Clinical Characteristics and Risk of Esophageal Squamous Neoplasia. Am J Gastroenterol. 2021;116(7):1533-1536. https://doi.org/10.14309/ajg.0000000000001225
Ravi K, Codipilly DC, Sunjaya D, Fang H, Arora AS, Katzka DA. Esophageal Lichen Planus Is Associated With a Significant Increase in Risk of Squamous Cell Carcinoma. Clin Gastroenterol Hepatol. 2019;17(9):1902-1903.e1. https://doi.org/10.1016/j.cgh.2018.10.018
Leeuwenburgh I, Scholten P, Alderliesten J, Tilanus HW, Looman CW, Steijerberg EW, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010;105(10):2144-9. https://doi.org/10.1038/ajg.2010.263
Sang HM, Cao JL, Soyfoo MD, Zhang WM, Jiang JX, Xu SF. Endoscopic and Histopathology Characteristics in Patients with Esophageal High-Grade Intraepithelial Neoplasia. Dig Surg. 2019;36(5):384-393. https://doi.org/10.1159/000490112
Singhi AD, Arnold CA, Lam-Himlin DM, Nikiforova MN, Voltaggio L, Canto MI, et al. Targeted next-generation sequencing supports epidermoid metaplasia of the esophagus as a precursor to esophageal squamous neoplasia. Mod Pathol. 2017;30(11):1613-1621. https://doi.org/10.1038/modpathol.2017.73
Ezoe Y, Fujii S, Muto M, Ochiai A, Ohtsu A. Epidermoid metaplasia of the esophagus: endoscopic feature and differential diagnosis. Hepatogastroenterology. 2011;58(107-108):809-13.
Aida J, Kobayashi T, Saku T, Yamaguchi M, Shimomura N, Nakamura K, et al. Short telomeres in an oral precancerous lesion: Q-FISH analysis of leukoplakia. J Oral Pathol Med. 2012;41(5):372-8. https://doi.org/10.1111/j.1600-0714.2011.01120.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















