Association Between Polycystic Ovary Syndrome and Fatty Liver Disease in Women: A Literature Review
DOI:
https://doi.org/10.22516/25007440.1238Keywords:
Nonalcoholic fatty liver disease, polycystic ovary syndrome, insulin resistance, Obesity Management, hyperandrogenismAbstract
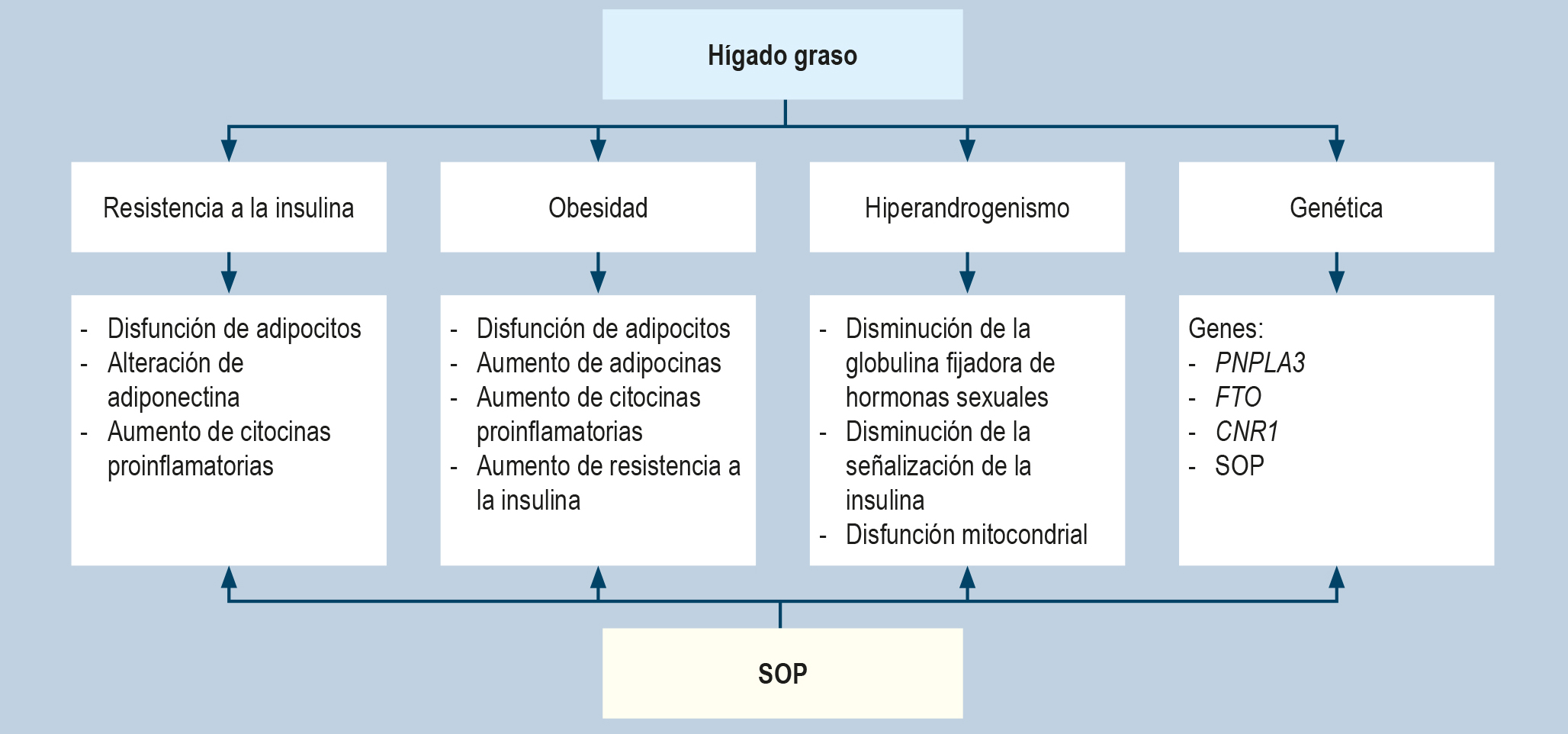
Introduction: Metabolic dysfunction-associated fatty liver disease (MAFLD) is a multisystem condition with a spectrum that begins with simple steatosis, followed by nonalcoholic steatohepatitis, and may progress to fibrosis. Its prevalence among women with polycystic ovary syndrome (PCOS) ranges from 34% to 70%, a relationship explained pathophysiologically by insulin resistance, obesity, hyperandrogenism, and other contributing factors. Currently, there is no approved treatment for either condition; therefore, management should focus on lifestyle modifications, including proper nutrition, weight loss, and physical activity—either as stand-alone strategies or in combination with pharmacological therapy.
Materials and methods: This article reviews current evidence on the association between fatty liver disease and PCOS. A literature search was conducted using DeCS and MeSH terms in both Spanish and English, including studies published from 2014 to date.
Conclusion: It is recommended that all women with PCOS undergo liver function testing and imaging studies (such as ultrasound and elastography) for the diagnosis of MAFLD.
Downloads
References
Cusi K, Isaacs S, Barb D, Basu R, Caprio S, Garvey WT, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract. 2022;28(5):528-562. https://doi.org/10.1016/j.eprac.2022.03.010
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84. https://doi.org/10.1002/hep.28431
Sadeghi HM, Adeli I, Calina D, Docea AO, Mousavi T, Daniali M, et al. Polycystic Ovary Syndrome: A Comprehensive Review of Pathogenesis, Management, and Drug Repurposing. Int J Mol Sci. 2022;23(2):583. https://doi.org/10.3390/ijms23020583
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology. 2023;78(6):1966-1986. https://doi.org/10.1097/HEP.0000000000000520
Hagström H, Vessby J, Ekstedt M, Shang Y. 99% of patients with NAFLD meet MASLD criteria and natural history is therefore identical. J Hepatol. 2024;80(2):e76-e77. https://doi.org/10.1016/j.jhep.2023.08.026
Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS, et al. Polycystic ovary syndrome. Nat Rev Dis Primers. 2016;2:16057. https://doi.org/10.1038/nrdp.2016.57
McCartney CR, Marshall JC. Clinical Practice. Polycystic Ovary Syndrome. N Engl J Med. 2016;375(1):54-64. https://doi.org/10.1056/NEJMcp1514916
Cerda C, Pérez-Ayuso RM, Riquelme A, Soza A, Villaseca P, Sir-Petermann T, et al. Nonalcoholic fatty liver disease in women with polycystic ovary syndrome. J Hepatol. 2007;47(3):412-7. https://doi.org/10.1016/j.jhep.2007.04.012
Rocha ALL, Faria LC, Guimarães TCM, Moreira GV, Cândido AL, Couto CA, et al. Non-alcoholic fatty liver disease in women with polycystic ovary syndrome: systematic review and meta-analysis. J Endocrinol Invest. 2017;40(12):1279-1288. https://doi.org/10.1007/s40618-017-0708-9
Xu Q, Zhang J, Lu Y, Wu L. Association of metabolic-dysfunction associated steatotic liver disease with polycystic ovary syndrome. iScience. 2024;27(2):108783. https://doi.org/10.1016/j.isci.2024.108783
Falzarano C, Lofton T, Osei-Ntansah A, Oliver T, Southward T, Stewart S, et al. Nonalcoholic Fatty Liver Disease in Women and Girls With Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2022;107(1):258-272. https://doi.org/10.1210/clinem/dgab658
Vassilatou E, Lafoyianni S, Vryonidou A, Ioannidis D, Kosma L, Katsoulis K, et al. Increased androgen bioavailability is associated with non-alcoholic fatty liver disease in women with polycystic ovary syndrome. Hum Reprod. 2010;25(1):212-20. https://doi.org/10.1093/humrep/dep380
Petersen MC, Madiraju AK, Gassaway BM, Marcel M, Nasiri AR, Butrico G, et al. Insulin receptor Thr1160 phosphorylation mediates lipid-induced hepatic insulin resistance. J Clin Invest. 2016;126(11):4361-4371. https://doi.org/10.1172/JCI86013
Khan RS, Bril F, Cusi K, Newsome PN. Modulation of Insulin Resistance in Nonalcoholic Fatty Liver Disease. Hepatology. 2019;70(2):711-724. https://doi.org/10.1002/hep.30429
Apridonidze T, Essah PA, Iuorno MJ, Nestler JE. Prevalence and characteristics of the metabolic syndrome in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2005;90(4):1929-35. https://doi.org/10.1210/jc.2004-1045
Moghetti P, Tosi F. Insulin resistance and PCOS: chicken or egg? J Endocrinol Invest. 2021;44(2):233-244. https://doi.org/10.1007/s40618-020-01351-0
Corbould A, Kim YB, Youngren JF, Pender C, Kahn BB, Lee A, et al. Insulin resistance in the skeletal muscle of women with PCOS involves intrinsic and acquired defects in insulin signaling. Am J Physiol Endocrinol Metab. 2005;288(5):E1047-54. https://doi.org/10.1152/ajpendo.00361.2004
Qu Z, Zhu Y, Jiang J, Shi Y, Chen Z. The clinical characteristics and etiological study of nonalcoholic fatty liver disease in Chinese women with PCOS. Iran J Reprod Med. 2013;11(9):725-32.
Karoli R, Fatima J, Chandra A, Gupta U, Islam FU, Singh G. Prevalence of hepatic steatosis in women with polycystic ovary syndrome. J Hum Reprod Sci. 2013;6(1):9-14. https://doi.org/10.4103/0974-1208.112370
Makri E, Goulas A, Polyzos SA. Epidemiology, Pathogenesis, Diagnosis and Emerging Treatment of Nonalcoholic Fatty Liver Disease. Arch Med Res. 2021;52(1):25-37. https://doi.org/10.1016/j.arcmed.2020.11.010
Lim SS, Davies MJ, Norman RJ, Moran LJ. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(6):618-37. https://doi.org/10.1093/humupd/dms030
Rodriguez Paris V, Solon-Biet SM, Senior AM, Edwards MC, Desai R, Tedla N, et al. Defining the impact of dietary macronutrient balance on PCOS traits. Nat Commun. 2020;11(1):5262. https://doi.org/10.1038/s41467-020-19003-5
Robker RL, Akison LK, Bennett BD, Thrupp PN, Chura LR, Russell DL, et al. Obese women exhibit differences in ovarian metabolites, hormones, and gene expression compared with moderate-weight women. J Clin Endocrinol Metab. 2009;94(5):1533-40. https://doi.org/10.1210/jc.2008-2648
Tantanavipas S, Vallibhakara O, Sobhonslidsuk A, Phongkitkarun S, Vallibhakara SA, Promson K, et al. Abdominal Obesity as a Predictive Factor of Nonalcoholic Fatty Liver Disease Assessed by Ultrasonography and Transient Elastography in Polycystic Ovary Syndrome and Healthy Women. Biomed Res Int. 2019;2019:9047324. https://doi.org/10.1155/2019/9047324
Petta S, Ciresi A, Bianco J, Geraci V, Boemi R, Galvano L, et al. Insulin resistance and hyperandrogenism drive steatosis and fibrosis risk in young females with PCOS. PLoS One. 2017;12(11):e0186136. https://doi.org/10.1371/journal.pone.0186136
Rodriguez Paris V, Bertoldo MJ. The Mechanism of Androgen Actions in PCOS Etiology. Med Sci (Basel). 2019;7(9):89. https://doi.org/10.3390/medsci7090089
Urbano F, Chiarito M, Lattanzio C, Messa A, Ferrante M, Francavilla M, et al. Sex Hormone-Binding Globulin (SHBG) Reduction: The Alarm Bell for the Risk of Non-Alcoholic Fatty Liver Disease in Adolescents with Polycystic Ovary Syndrome. Children (Basel). 2022;9(11):1748. https://doi.org/10.3390/children9111748
Luo J, Chen Q, Shen T, Wang X, Fang W, Wu X, et al. Association of sex hormone-binding globulin with nonalcoholic fatty liver disease in Chinese adults. Nutr Metab (Lond). 2018;15:79. https://doi.org/10.1186/s12986-018-0313-8
Feng C, Jin Z, Chi X, Zhang B, Wang X, Sun L, et al. SHBG expression is correlated with PI3K/AKT pathway activity in a cellular model of human insulin resistance. Gynecol Endocrinol. 2018;34(7):567-573. https://doi.org/10.1080/09513590.2017.1411474
Malini NA, Roy George K. Evaluation of different ranges of LH:FSH ratios in polycystic ovarian syndrome (PCOS) - Clinical based case control study. Gen Comp Endocrinol. 2018;260:51-57. https://doi.org/10.1016/j.ygcen.2017.12.007
Hong SH, Sung YA, Hong YS, Song DK, Jung H, Jeong K, et al. Non-alcoholic fatty liver disease is associated with hyperandrogenism in women with polycystic ovary syndrome. Sci Rep. 2023;13(1):13397. https://doi.org/10.1038/s41598-023-39428-4
Kim JJ, Kim D, Yim JY, Kang JH, Han KH, Kim SM, et al. Polycystic ovary syndrome with hyperandrogenism as a risk factor for non-obese non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2017;45(11):1403-1412. https://doi.org/10.1111/apt.14058
Jensen T, Abdelmalek MF, Sullivan S, Nadeau KJ, Green M, Roncal C, et al. Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68(5):1063-1075. https://doi.org/10.1016/j.jhep.2018.01.019
Singla R, Gupta Y, Khemani M, Aggarwal S. Thyroid disorders and polycystic ovary syndrome: An emerging relationship. Indian J Endocrinol Metab. 2015;19(1):25-9. https://doi.org/10.4103/2230-8210.146860
Gao H, Lu X, Huang H, Ji H, Zhang L, Su Z. Thyroid-stimulating hormone level is negatively associated with fertilization rate in patients with polycystic ovary syndrome undergoing in vitro fertilization. Int J Gynaecol Obstet. 2021;155(1):138-145. https://doi.org/10.1002/ijgo.13581
Kim D, Vazquez-Montesino LM, Escober JA, Fernandes CT, Cholankeril G, Loomba R, et al. Low Thyroid Function in Nonalcoholic Fatty Liver Disease Is an Independent Predictor of All-Cause and Cardiovascular Mortality. Am J Gastroenterol. 2020;115(9):1496-1504. https://doi.org/10.14309/ajg.0000000000000654
Matias I, Gatta-Cherifi B, Cota D. Obesity and the Endocannabinoid System: Circulating Endocannabinoids and Obesity. Current Obesity Reports. 2012;1(4):229-35. https://doi.org/10.1007/s13679-012-0027-6
Jędrzejuk D, Laczmański L, Kuliczkowska J, Lenarcik A, Trzmiel-Bira A, Hirnle L, et al. Selected CNR1 polymorphisms and hyperandrogenemia as well as fat mass and fat distribution in women with polycystic ovary syndrome. Gynecol Endocrinol. 2015;31(1):36-9. https://doi.org/10.3109/09513590.2014.946899
Dawson AJ, Kilpatrick ES, Coady AM, Elshewehy AMM, Dakroury Y, Ahmed L, et al. Endocannabinoid receptor blockade reduces alanine aminotransferase in polycystic ovary syndrome independent of weight loss. BMC Endocr Disord. 2017;17(1):41. https://doi.org/10.1186/s12902-017-0194-2
Hoeger KM, Dokras A, Piltonen T. Update on PCOS: Consequences, Challenges, and Guiding Treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083. https://doi.org/10.1210/clinem/dgaa839
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19-25. https://doi.org/10.1016/j.fertnstert.2003.10.004
Azziz R. Polycystic Ovary Syndrome. Obstet Gynecol. 2018;132(2):321-336. https://doi.org/10.1097/AOG.0000000000002698
Chen MJ, Ho HN. Hepatic manifestations of women with polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2016;37:119-128. https://doi.org/10.1016/j.bpobgyn.2016.03.003
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202-209. https://doi.org/10.1016/j.jhep.2020.03.039
Vassilatou E. Nonalcoholic fatty liver disease and polycystic ovary syndrome. World J Gastroenterol. 2014;20(26):8351-63. https://doi.org/10.3748/wjg.v20.i26.8351
Spremović Rađenović S, Pupovac M, Andjić M, Bila J, Srećković S, Gudović A, et al. Prevalence, Risk Factors, and Pathophysiology of Nonalcoholic Fatty Liver Disease (NAFLD) in Women with Polycystic Ovary Syndrome (PCOS). Biomedicines. 2022;10(1):131. https://doi.org/10.3390/biomedicines10010131
Ferraioli G, Soares Monteiro LB. Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol. 2019;25(40):6053-6062. https://doi.org/10.3748/wjg.v25.i40.6053
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55(6):2005-23. https://doi.org/10.1002/hep.25762
Vidal-Cevallos P, Mijangos-Trejo A, Uribe M, Tapia NC. The Interlink Between Metabolic-Associated Fatty Liver Disease and Polycystic Ovary Syndrome. Endocrinol Metab Clin North Am. 2023;52(3):533-545. https://doi.org/10.1016/j.ecl.2023.01.005
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602-1618. https://doi.org/10.1093/humrep/dey256
European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the Management of Non-Alcoholic Fatty Liver Disease. Obes Facts. 2016;9(2):65-90. https://doi.org/10.1159/000443344
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149(2):367-78.e5. ttps://doi.org/10.1053/j.gastro.2015.04.005
Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829-846. https://doi.org/10.1016/j.jhep.2017.05.016
Zhang CS, Li M, Ma T, Zong Y, Cui J, Feng JW, et al. Metformin Activates AMPK through the Lysosomal Pathway. Cell Metab. 2016;24(4):521-522. https://doi.org/10.1016/j.cmet.2016.09.003
Kristensen JM, Treebak JT, Schjerling P, Goodyear L, Wojtaszewski JF. Two weeks of metformin treatment induces AMPK-dependent enhancement of insulin-stimulated glucose uptake in mouse soleus muscle. Am J Physiol Endocrinol Metab. 2014;306(10):E1099-109. https://doi.org/10.1152/ajpendo.00417.2013
Rakoski MO, Singal AG, Rogers MA, Conjeevaram H. Meta-analysis: insulin sensitizers for the treatment of non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2010;32(10):1211-21. https://doi.org/10.1111/j.1365-2036.2010.04467.x
Siamashvili M, Davis SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2021;14(9):1081-1089. https://doi.org/10.1080/17512433.2021.1933433
Patel Chavez C, Cusi K, Kadiyala S. The Emerging Role of Glucagon-like Peptide-1 Receptor Agonists for the Management of NAFLD. J Clin Endocrinol Metab. 2022;107(1):29-38. https://doi.org/10.1210/clinem/dgab578
Cusi K. Incretin-Based Therapies for the Management of Nonalcoholic Fatty Liver Disease in Patients With Type 2 Diabetes. Hepatology. 2019;69(6):2318-2322. https://doi.org/10.1002/hep.30670
Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. N Engl J Med. 2021;384(12):1113-1124. https://doi.org/10.1056/NEJMoa2028395
Cena H, Chiovato L, Nappi RE. Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab. 2020;105(8):e2695–709. https://doi.org/10.1210/clinem/dgaa285
Frøssing S, Nylander M, Chabanova E, Frystyk J, Holst JJ, Kistorp C, et al. Effect of liraglutide on ectopic fat in polycystic ovary syndrome: A randomized clinical trial. Diabetes Obes Metab. 2018;20(1):215-218. https://doi.org/10.1111/dom.13053
Kuchay MS, Krishan S, Mishra SK, Farooqui KJ, Singh MK, Wasir JS, et al. Effect of Empagliflozin on Liver Fat in Patients With Type 2 Diabetes and Nonalcoholic Fatty Liver Disease: A Randomized Controlled Trial (E-LIFT Trial). Diabetes Care. 2018;41(8):1801-1808. https://doi.org/10.2337/dc18-0165
Javed Z, Papageorgiou M, Deshmukh H, Rigby AS, Qamar U, Abbas J, et al. Effects of empagliflozin on metabolic parameters in polycystic ovary syndrome: A randomized controlled study. Clin Endocrinol (Oxf). 2019;90(6):805-813. https://doi.org/10.1111/cen.13968
Yaribeygi H, Maleki M, Butler AE, Jamialahmadi T, Sahebkar A. New insights into cellular links between sodium-glucose cotransporter-2 inhibitors and ketogenesis. J Cell Biochem. 2022;123(12):1879-1890. https://doi.org/10.1002/jcb.30327
Rotman Y, Sanyal AJ. Current and upcoming pharmacotherapy for non-alcoholic fatty liver disease. Gut. 2017;66(1):180-190. https://doi.org/10.1136/gutjnl-2016-312431
Moran LJ, Tassone EC, Boyle J, Brennan L, Harrison CL, Hirschberg AL, et al. Evidence summaries and recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome: Lifestyle management. Obes Rev. 2020;21(10):e13046. https://doi.org/10.1111/obr.13046
Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007;370(9588):685-97. https://doi.org/10.1016/S0140-6736(07)61345-2
Collée J, Mawet M, Tebache L, Nisolle M, Brichant G. Polycystic ovarian syndrome and infertility: overview and insights of the putative treatments. Gynecol Endocrinol. 2021;37(10):869-874. https://doi.org/10.1080/09513590.2021.1958310
Balen AH, Morley LC, Misso M, Franks S, Legro RS, Wijeyaratne CN, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016;22(6):687-708. https://doi.org/10.1093/humupd/dmw025
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















