Association Between Ulcerative Colitis and Pulmonary Embolism: A Case Report
DOI:
https://doi.org/10.22516/25007440.1208Keywords:
Ulcerative colitis, pulmonary embolism, inflammatory bowel disease, inflammation, coagulationAbstract
Introduction: Inflammatory bowel diseases (IBD) include Crohn’s disease (CD) and ulcerative colitis (UC), conditions that primarily affect the intestines but can sometimes lead to extraintestinal complications such as venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE).
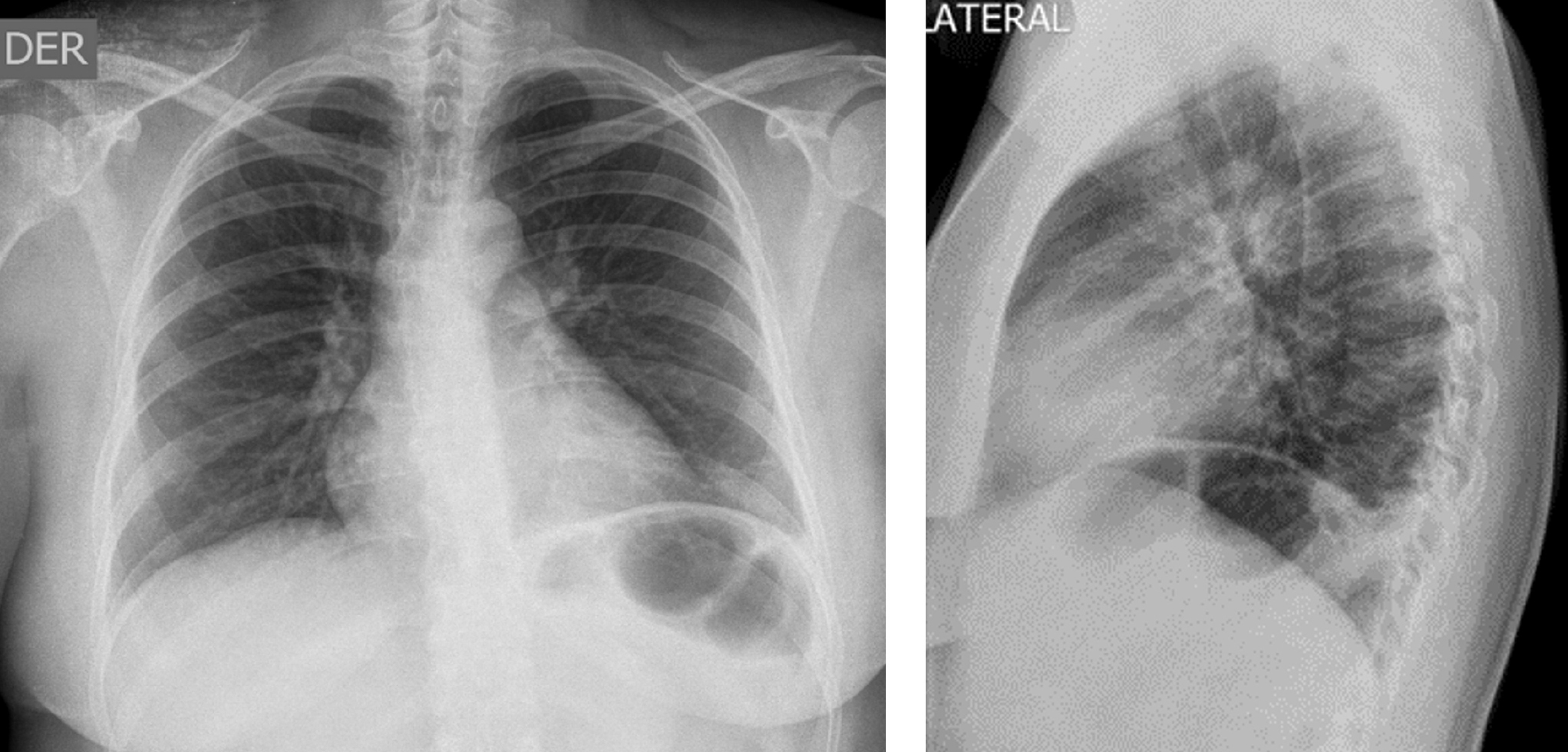
Case Report: A 39-year-old woman was admitted with a 12-hour history of left-sided chest pain radiating to the ipsilateral scapular region, worsened by breathing and positional changes. She reported a prior episode of deep vein thrombosis in her right leg. Laboratory tests revealed microcytic hypochromic anemia and thrombocytosis. Imaging studies showed findings suggestive of pulmonary infarction, with a CT pulmonary angiogram confirming a thrombus at the segmental branch of the right lower lobe, accompanied by right-sided pleural effusion and atelectasis. Further evaluation for anemia, including a colonoscopy, revealed acute-phase pancolitis with minimal bleeding. An autoimmune panel was negative. Treatment was initiated with anticoagulation, mesalazine, and methylprednisolone.
Conclusions: Thromboembolic complications occur in approximately 1% to 8% of patients presenting with active inflammatory bowel disease and are associated with increased morbidity and mortality. The underlying pathophysiological mechanisms likely involve a hypercoagulable state, platelet aggregation, impaired fibrinolysis, and genetic predisposition. Identifying risk factors and implementing appropriate therapeutic measures are crucial to preventing future thromboembolic events. The preferred prophylactic anticoagulation therapy is low-molecular-weight heparin, which is recommended for hospitalized patients at high risk during active disease phases.
Downloads
References
Danese S, Papa A, Saibeni S, Repici A, Malesci A, Vecchi M. Inflammation and coagulation in inflammatory bowel disease: The clot thickens. Am J Gastroenterol. 2007;102(1):174-86. https://doi.org/10.1111/j.1572-0241.2006.00943.x
Bergen J.A Barker N.W Extensive arterial and venous thrombosis complicating chronic ulcerative colitis. Arch Intern Med (Chic). 1936;58(1):17-31. https://doi.org/10.1001/archinte.1936.00170110025002
Murthy SK, Nguyen GC. Venous thromboembolism in inflammatory bowel disease: an epidemiological review. Am J Gastroenterol. 2011;106(4):713-8. https://doi.org/10.1038/ajg.2011.53
Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. Long-term complications, extraintestinal manifestations, and mortality in adult Crohn’s disease in population-based cohorts. Inflamm Bowel Dis. 2011;17(1):471-8. https://doi.org/10.1002/ibd.21417
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685-95. https://doi.org/10.1056/NEJMra043430
Gamarra V, Amaya N, Vásquez G, Mora E, Donet J. Trombosis venosa profunda como manifestación extra intestinal de colitis ulcerativa: presentación de un caso. Rev Gastroenterol Perú. 2012;32(2):192-196.
Tan VP, Chung A, Yan BP, Gibson PR. Venous and arterial disease in inflammatory bowel disease. J Gastroenterol Hepatol. 2013;28(7):1095-1113. https://doi.org/10.1111/jgh.12260
Alatri A, Schoepfer A, Fournier N, Engelberger R, Safroneeva E, Vavricka S, et al. Prevalence and risk factors for venous thromboembolic complications in the Swiss Inflammatory Bowel Disease Cohort. Scand J Gastroenterol. 2016;51(10):1200-5. https://doi.org/10.1080/00365521.2016.1185464
Tajdini M, Hosseini SM. From Pulmonary Embolism to Inflammatory Bowel Disease; Give Tunnel Vision up. Emerg (Tehran). 2016;4(1):41-4.
Cheng K, Faye AS. Venous thromboembolism in inflammatory bowel disease. World J Gastroenterol. 2020;26(12):1231-1241. https://doi.org/10.3748/wjg.v26.i12.1231
Suárez C, Vera M, San Román L, Gonzáles Y, Calvo M, García M, et al. Riesgo de fenómenos tromboembólicos en pacientes con enfermedad inflamatoria intestinal. Gastroenterol Hepatol. 2012;35(9):634-639. https://doi.org/10.1016/j.gastrohep.2012.07.003
Giannotta M, Tapete G, Emmi G, Silvestri E, Milla M. Thrombosis in inflammatory bowel diseases: what’s the link?. Thromb J. 2015;13:14. https://doi.org/10.1186/s12959-015-0044-2
Campos A, Ramírez P, Ganchegui I, Urtasun L, Sánchez A, Spicakova K, et al. Tromboembólicas en enfermedad inflamatoria intestinal. Enferm Inflam Intest Dia. 2015;14(3):81-86. https://doi.org/10.1016/j.eii.2015.08.002
Baños Madrid R, Salama Benarroch H, Martínez Crespo J, Morán Sánchez S, Vargas Acosta A, Mercader Martínez J. Vascular complications associated with inflammatory bowel disease. An Med Interna (Madrid). 2003;20(2):33-36. https://doi.org/10.4321/S0212-71992003000200008
Kim J, Cheon J. Pathogenesis and clinical perspectives of extraintestinal manifestations in inflammatory bowel diseases. Intest Res. 2020;18(3):249-264. https://doi.org/10.5217/ir.2019.00128
Papa A, Gerardi V, Marzo M, Felice C, Rapaccini GL, Gasbarrini A. Venous thromboembolism in patients with inflammatory bowel disease: focus on prevention and treatment. World J Gastroenterol. 2014;20(12):3173-3179. https://doi.org/10.3748/wjg.v20.i12.3173
Bryant R, Jairath V, Curry N, Travis S. Thrombosis in inflammatory bowel disease: Are we tailoring prophylaxis to those most at risk? J Crohns Colitis. 2014;8(2):166-171. https://doi.org/10.1016/j.crohns.2013.09.007
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















