Morbidity and Mortality in COVID-19 Patients With and Without Gastrointestinal Symptoms
DOI:
https://doi.org/10.22516/25007440.1051Keywords:
COVID 19, Clinical symptoms, Intensive Care Unit, Mechanical Ventilation, Mortality, Bacterial InfectionsAbstract
Objective: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) causes a wide range of symptoms, including gastrointestinal manifestations such as nausea, vomiting, diarrhea, and abdominal pain. This study aimed to evaluate whether the presence or absence of these gastrointestinal symptoms could be associated with more severe disease progression, defined as death, the need for intensive care unit (ICU) management, mechanical ventilation, or bacterial coinfection.
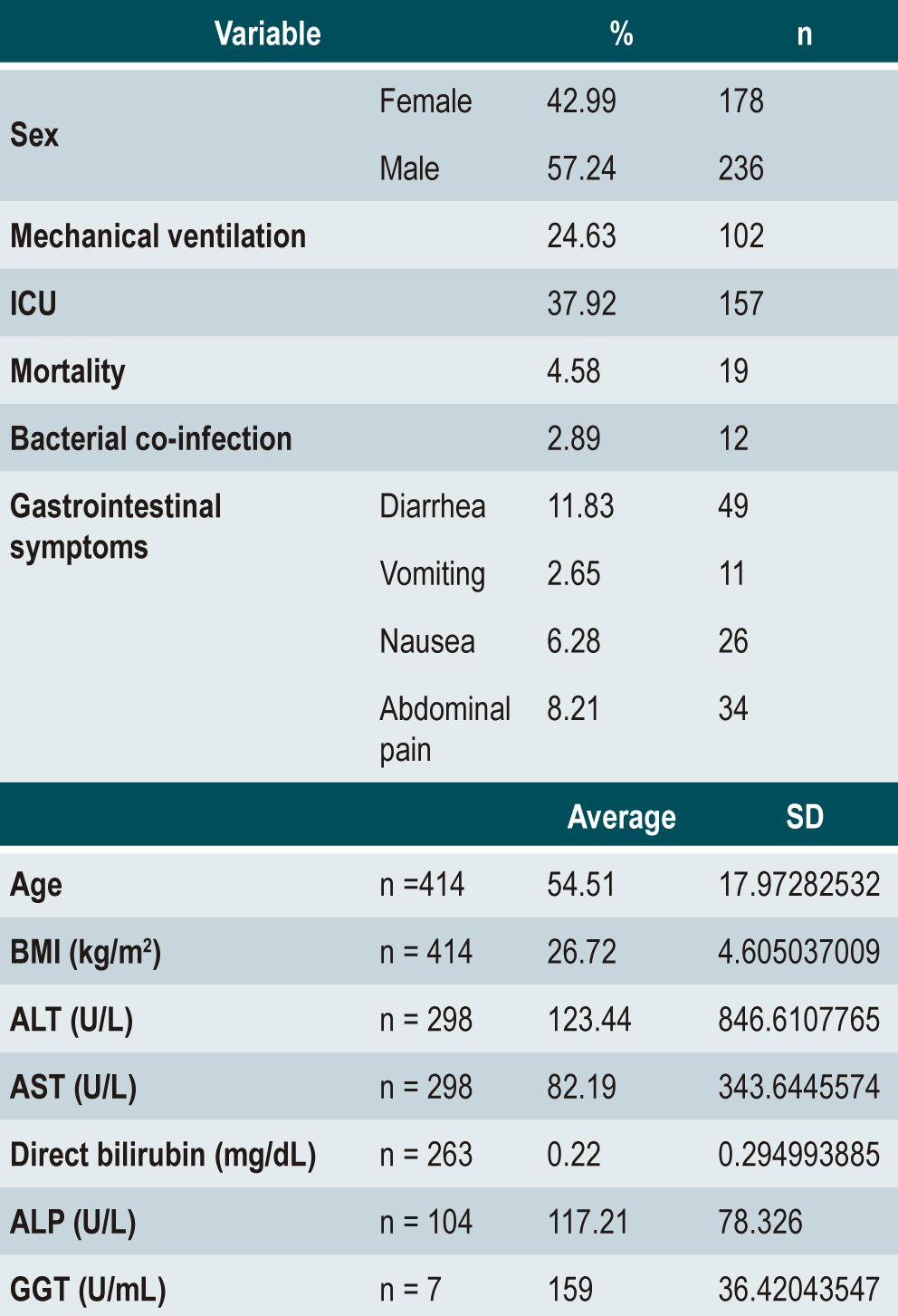
Patients and Methods: An analytical observational cohort study was conducted with confirmed COVID-19 patients with gastrointestinal symptoms and a comparison group without gastrointestinal symptoms. Patients included were over 18 years old, presented with symptoms suggestive of COVID-19, and had the diagnosis confirmed by a polymerase chain reaction test.
Results: A total of 414 patients who met the selection criteria were analyzed, and it was found that mortality was influenced only by age, while mechanical ventilation and the need for ICU management were related to liver function profile. However, no difference in severity was found between patients with gastrointestinal symptoms and those without.
Conclusions: Gastrointestinal symptoms alone do not represent a risk for the progression of SARS-CoV-2 disease, however, levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and direct bilirubin (DB) should be included in the initial assessment of these patients, as they provide prognostic value according to the results of our study.
Downloads
References
World Health Organization. COVID-19 cases | WHO COVID-19 dashboard [Internet]. Datadot [consultado el 30 de noviembre de 2021]. Disponible en: https://covid19.who.int/
Johns Hopkins Coronavirus Resource Center. COVID-19 Map - Johns Hopkins Coronavirus Resource Center [Internet]. Johns Hopkins Coronavirus Resource Center [consultado el 30 de noviembre de 2021]. Disponible en: https://coronavirus.jhu.edu/map.html
Sierra-Arango F, Vergara-Cabra C, Vásquez-Roldan M, Pérez-Riveros ED. Acute surgical‐like abdomen as a gastrointestinal manifestation of COVID-19 infection: a case report in Colombia. BMC Gastroenterol. 2021;21(1):187. https://doi.org/10.1186/s12876-021-01762-0
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33. https://doi.org/10.1056/NEJMoa2001017
Ministerio de Salud y Protección Social. Así va el aplanamiento de la curva epidemiológica en el país [Internet]. Ministerio de Salud y Protección Social [consultado el 30 de noviembre de 2021]. Disponible en: https://www.minsalud.gov.co/Paginas/Asi-va-el-aplanamiento-de-la-curva-epidemiologica-en-el-pais-.aspx
Instituto Nacional de Salud. Coronavirus Colombia [Internet]. Instituto Nacional de Salud [consultado el 30 de noviembre de 2021]. Disponible en: https://www.ins.gov.co/Noticias/paginas/coronavirus.aspx
Azwar MK, Kirana F, Kurniawan A, Handayani S, Setiati S. Gastrointestinal Presentation in COVID-19 in Indonesia: A Case Report. Acta Medica Indones. 2020;52(1):63-7.
Nobel YR, Phipps M, Zucker J, Lebwohl B, Wang TC, Sobieszczyk ME, et al. Gastrointestinal Symptoms and Coronavirus Disease 2019: A Case-Control Study From the United States. Gastroenterology. 2020;159(1):373-375.e2. https://doi.org/10.1053/j.gastro.2020.04.017
Suresh Kumar VC, Mukherjee S, Harne PS, Subedi A, Ganapathy MK, Patthipati VS, et al. Novelty in the gut: a systematic review and meta-analysis of the gastrointestinal manifestations of COVID-19. BMJ Open Gastroenterol. 2020;7(1):e000417. https://doi.org/10.1136/bmjgast-2020-000417
Dong Z, Xiang B-J, Jiang M, Sun M, Dai C. The Prevalence of Gastrointestinal Symptoms, Abnormal Liver Function, Digestive System Disease and Liver Disease in COVID-19 Infection: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2021;55(1):67-76. https://doi.org/10.1097/MCG.0000000000001424
Wong SH, Lui RN, Sung JJ. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35(5):744-8. https://doi.org/10.1111/jgh.15047
Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667-678. https://doi.org/10.1016/S2468-1253(20)30126-6
World Medical Association. Declaración de Helsinki de la AMM – Principios éticos para las investigaciones médicas en seres humanos [Internet]. The World Medical Association [consultado el 30 de noviembre de 2021]. Disponible en: https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/
Ministerio de Salud y Protección Social. Resolución 8430 de 1993, por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud [Internet]. Ministerio de Salud y Protección Social [consultado el 30 de noviembre de 2021]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.PDF
Jin X, Lian J-S, Hu J-H, Gao J, Zheng L, Zhang Y-M, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002-1009. https://doi.org/10.1136/gutjnl-2020-320926
Tariq R, Saha S, Furqan F, Hassett L, Pardi D, Khanna S. Prevalence and Mortality of COVID-19 Patients With Gastrointestinal Symptoms: A Systematic Review and Meta-analysis. Mayo Clin Proc. 2020;95(8):1632-1648. https://doi.org/10.1016/j.mayocp.2020.06.003
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. https://doi.org/10.1001/jama.2020.1585
Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51(9):843–51. https://doi.org/10.1111/apt.15731
Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, et al. COVID-19: Abnormal liver function tests. J Hepatol. 2020;73(3):566-74. https://doi.org/10.1016/j.jhep.2020.04.006
Gul F, Lo KB, Peterson J, McCullough PA, Goyal A, Rangaswami J. Meta-analysis of outcomes of patients with COVID-19 infection with versus without gastrointestinal symptoms. Bayl Univ Med Cent Proc. 2020;33(3):366-9. https://doi.org/10.1080/08998280.2020.1771164
Wang H, Qiu P, Liu J, Wang F, Zhao Q. The liver injury and gastrointestinal symptoms in patients with Coronavirus Disease 19: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2020;44(5):653-661. https://doi.org/10.1016/j.clinre.2020.04.012
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















