Low-Dose Ketamine in Combination with Midazolam for Diagnostic Upper Gastrointestinal Endoscopy: Case Report
DOI:
https://doi.org/10.22516/25007440.1226Keywords:
Gastrointestinal endoscopy, conscious sedation, ketamine, midazolan, safetyAbstract
Introduction and objectives: The number of outpatient endoscopic procedures in gastroenterology has increased in recent years. During the pandemic, due to drug shortages, alternative sedation techniques were explored. This study describes the sedation profile and adverse effects of combining low-dose ketamine with midazolam for sedation during diagnostic upper gastrointestinal endoscopy (UGIE).
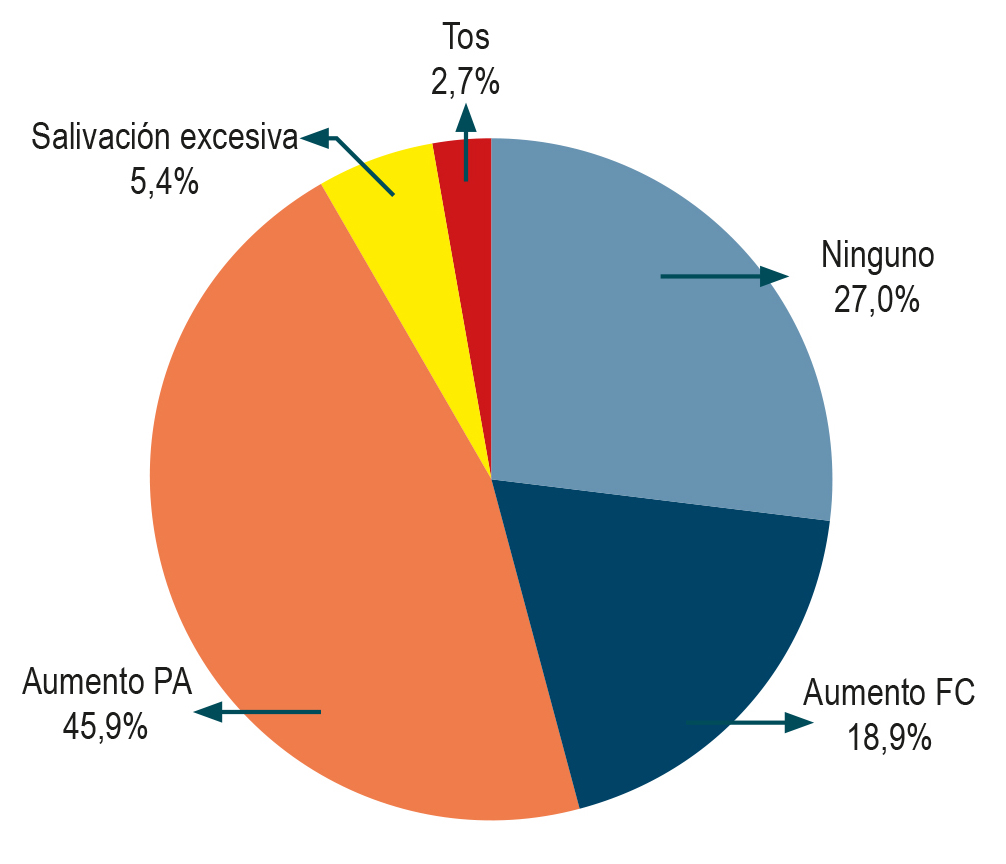
Materials and methods: A prospective, observational, descriptive case series study was conducted involving 30 patients aged 18 to 70 years with ASA physical status classification I or II, who underwent diagnostic UGIE. Sedation was induced with 0.03 mg/kg of midazolam and 0.3 mg/kg of ketamine prior to endoscopy. During and after endoscopy, the need for additional sedative medications and the occurrence of major adverse events (e.g., cardiorespiratory arrest or death) and minor events (e.g., desaturation, apnea, laryngospasm, hypertension, tachycardia, coughing, hypersalivation, dizziness, and recall of the procedure) were documented. Procedure duration, recovery time, and depth of sedation were also recorded.
Results: Effective sedation was achieved in 27 ASA I and II patients without the need for additional sedatives to achieve the endoscopic procedure. The mean procedure time was 7.9 minutes, and the average recovery time was 26.1 minutes. Adverse events were observed in 66% of patients during the procedure (the most frequent being elevated blood pressure in 45.9%) and in 63.4% during recovery (most commonly dizziness in 50%).
Conclusions: The combination of low-dose ketamine and midazolam appears to be a safe and effective sedation strategy for diagnostic UGIE, with minor adverse effects reported in more than 50% of patients.
Downloads
References
Ammar MA, Sacha GL, Welch SC, Bass SN, Kane-Gill SL, Duggal A, et al. Sedation, Analgesia, and Paralysis in COVID-19 Patients in the Setting of Drug Shortages. J Intensive Care Med. 2021;36(2):157-74. https://doi.org/10.1177/0885066620951426
Shuman AG, Fox E, Unguru Y. Preparing for COVID-19-related Drug Shortages. Ann Am Thorac Soc. 2020;17(8):928-31. https://doi.org/10.1513/AnnalsATS.202004-362VP
Goudra B, Singh P. Propofol alternatives in gastrointestinal endoscopy anesthesia. Saudi J Anaesth. 2014;8(4):540-546. https://doi.org/10.4103/1658-354X.140893
Sleigh J, Harvey M, Voss L, Denny B. Ketamine - more mechanisms of action than just NMDA blockade. Trends in Anaesthesia and Critical Care. 2014;4(2-3):76-81. https://doi.org/10.1016/j.tacc.2014.03.002
Kurdi M, Theerth K, Deva R. Ketamine: Current applications in anesthesia, pain, and critical care. Anesth Essays Res. 2014;8(3):283-90. https://doi.org/10.4103/0259-1162.143110
Nowacka A, Borczyk M. Ketamine applications beyond anesthesia - A literature review. Eur J Pharmacol. 2019;860:172547. https://doi.org/10.1016/j.ejphar.2019.172547
Brecelj J, Kamhi Trop T, Orel R. Ketamine With and Without Midazolam for Gastrointestinal Endoscopies in Children. J Pediatr Gastroenterol Nutr. 2012;54(6):748-52. https://doi.org/10.1097/MPG.0b013e31824504af
Takzare A, Ebrahim Soltani A, Maleki A, Nooralishahi B, Kaheh F, Arab S, et al. Comparison of Propofol-Ketamine vs Propofol-Fentanyl for Pediatric Sedation during Upper Gastrointestinal Endoscopy. Arch Anesth & Crit Care. 2016;2(3):222-225.
Mogahed MM, Salama ER. A Comparison of Ketamine-Dexmedetomidine versus Ketamine-Propofol for Sedation in Children during Upper Gastrointestinal Endoscopy. J Anesth Clin Res 2017;8(11):1000785. https://doi.org/10.4172/2155-6148.1000785
Lightdale JR, Mitchell PD, Fredette ME, Mahoney LB, Zgleszewski SE, Scharff L, et al. A pilot study of ketamine versus midazolam/fentanyl sedation in children undergoing GI endoscopy. International Int J Pediatr. 2011;2011:623710. https://doi.org/10.1155/2011/623710
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.



















